
|
Developed by 
|
Supported by 

|
Bedaquiline
Developer(s)

|
Janssen Pharmaceuticals https://www.janssen.comBelgium Janssen Pharmaceuticals is a subsidiary company of Johnson & Johnson headquartered in Beerse, Belgium. They focus on manufacturing and developing pharmaceutical products for use in areas such as, Immunology, Infectious Diseases & Vaccines, Pulmonary Hypertension, Cardiovascular & Metabolism, Oncology, and Neuroscience. |
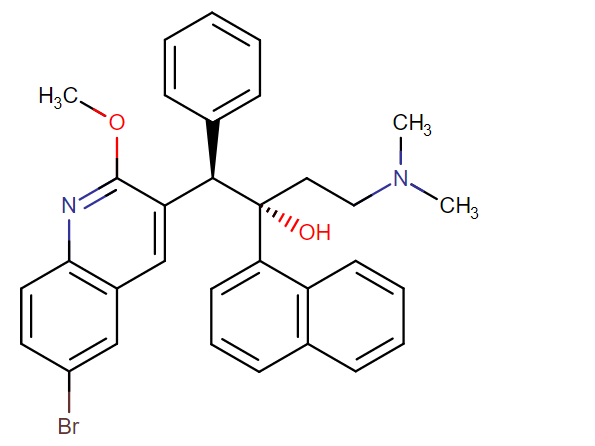
Drug structure
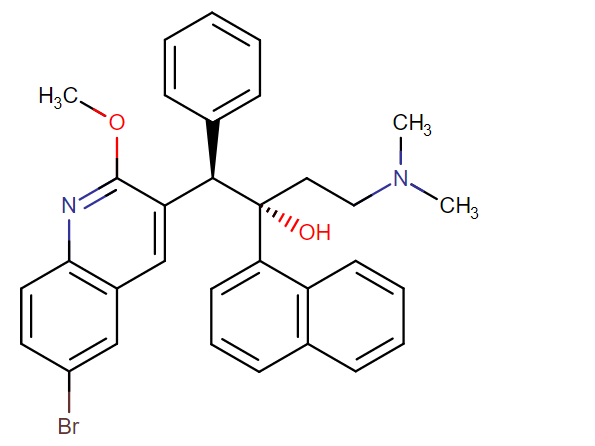
Bedaquiline Structure
Sourced from DrugBank
Drug information
Associated long-acting platforms
Polymer-based particles, In-situ forming gel/implant, Based on other organic particles
Administration route
Oral, Intramuscular, Subcutaneous, Intravenous
Therapeutic area(s)
Use case(s)
Use of drug
Ease of administration
Frequency of administration
Not provided
User acceptance
Not provided
Dosage
Available dose and strength
long acting formulation is being investigated
Maximum dose
Not provided
Recommended dosing regimen
Not provided
Additional comments
Not provided
Dosage link(s)
Not provided
Drug information
Drug's link(s)
Not provided
Generic name
Brand name
Compound type
Summary
Approval status
Regulatory authorities
Delivery device(s)
No delivery device
Scale-up and manufacturing prospects
Scale-up prospects
Formulations for long-acting Bedaquiline are currently in pre-clinical development, and therefore detailed scale-up information is unavailable. Several promising long-acting formulation approaches have been reported, including: (1) nanoemulsion-based chitosan nanocapsules, (2) lipid nanoparticles, and (3) a PLGA in-situ forming gel.
Tentative equipment list for manufacturing
Detailed information regarding industrial manufacturing requirements and/or equipment lists is currently not available as long-acting bedaquiline formulations have only been produced at small-scale for preclinical research use.
Manufacturing
Not provided
Specific analytical instrument required for characterization of formulation
Not provided
Clinical trials
A Single Ascending Dose, Single-Centre Study, to Assess Pharmacokinetics, Safety and Tolerability of a Single Intramuscular Dose of Bedaquiline Long-Acting Injection Formulation in Healthy Participants
Identifier
EUCT 2023-508810-41-00
Link
https://euclinicaltrials.eu/ctis-public/view/2023-508810-41-00?lang=en
Phase
Phase I
Status
Recruiting
Sponsor
Janssen Cilag International
More details
Not provided
Purpose
Safety and Tolerability of a Single Intramuscular Dose of Bedaquiline Long-Acting Injection Formulation
Interventions
Intervention 1
Countries
Sites / Institutions
Not provided
Trials dates
Anticipated Start Date
2024-06-03
Actual Start Date
2024-07-02
Anticipated Date of Last Follow-up
Not provided
Estimated Primary Completion Date
Not provided
Estimated Completion Date
2026-02-17
Actual Primary Completion Date
Not provided
Actual Completion Date
Not provided
Studied populations
Age Cohort
- Adults
Genders
- All
Accepts pregnant individuals
Unspecified
Accepts lactating individuals
Unspecified
Accepts healthy individuals
Yes
Comments about the studied populations
study protocol code: TMC207TBC1006
Health status
Study type
Interventional (clinical trial)
Enrollment
Not provided
Allocation
Non-randomized
Intervention model
Not provided
Intervention model description
Not provided
Masking
Open label
Masking description
Not provided
Frequency of administration
Studied LA-formulation(s)
Studied route(s) of administration
Use case
Treatment
Key resources
Excipients
Proprietary excipients used
Not provided
Novel excipients or existing excipients at a concentration above Inactive Ingredients Database (IID) for the specified route of administration
Not provided
Residual solvents used
Not provided
Patent info
Compound patent families
Patent informations
| Patent description | Representative patent | Categories | Patent holder | Licence with MPP | Patent source |
|---|---|---|---|---|---|
|
Bedaquiline Long-acting formulations (suspension of micro- or nanoparticles)
Expiry date: 2038-07-13 This invention concerns pharmaceutical compositions for administration via intramuscular or subcutaneous injection, comprising micro- or nanoparticles of the anti- TB compound bedaquiline, suspended in an aqueous pharmaceutically acceptable carrier, and the use of such pharmaceutical compositions in the treatment and prophylaxis of a pathogenic mycobacterial infection. |
WO2019012100 | Composition | Janssen Pharmaceutica Nv | No |
Patent status
| Patent status/countries | Low, Low- middle and upper-middle | High income |
|---|---|---|
| Granted | China, Kazakhstan, Morocco, Tunisia, Albania, Serbia, Bosnia and Herzegovina, Cambodia, Montenegro, Türkiye, North Macedonia, Jordan, Peru, Ukraine, South Africa, Sierra Leone, Eswatini, Liberia, Namibia, Sao Tome and Principe, Mozambique, Uganda, Zambia, Zimbabwe, Tanzania, United Republic of, Malawi, Ghana, Sudan, Botswana, Lesotho, Kenya, Gambia (the), Indonesia, Mexico, Nigeria, Congo, Mauritania, Guinea-Bissau, Niger, Senegal, Cameroon, Mali, Togo, Burkina Faso, Benin, Côte d'Ivoire, Central African Republic, Comoros, Guinea, Gabon, Equatorial Guinea, Chad, Viet Nam | Australia, Russian Federation, Liechtenstein, Italy, Norway, Malta, Denmark, Belgium, United Kingdom, Greece, Netherlands, Hungary, Croatia, Switzerland, Spain, San Marino, Slovenia, Austria, Romania, Iceland, Cyprus, Finland, France, Bulgaria, Slovakia, Poland, Latvia, Ireland, Estonia, Germany, Luxembourg, Portugal, Czechia, Lithuania, Monaco, Sweden, Japan, Korea, Republic of, Saudi Arabia, United States of America, Hong Kong |
| Filed | Brazil, China, Albania, Serbia, Türkiye, North Macedonia, Philippines, Papua New Guinea, Thailand, Uzbekistan | Canada, Liechtenstein, Italy, Norway, Malta, Denmark, Belgium, United Kingdom, Greece, Netherlands, Hungary, Croatia, Switzerland, Spain, San Marino, Slovenia, Austria, Romania, Iceland, Cyprus, Finland, France, Bulgaria, Slovakia, Poland, Latvia, Ireland, Estonia, Germany, Luxembourg, Portugal, Czechia, Lithuania, Monaco, Sweden, Kuwait, Qatar |
| Not in force | World Intellectual Property Organization (WIPO), Colombia, Tajikistan, Belarus, Azerbaijan, Turkmenistan, Armenia, Kyrgyzstan, Morocco, Tunisia, Bosnia and Herzegovina, Cambodia, Montenegro, Moldova, Republic of, India, Rwanda | World Intellectual Property Organization (WIPO), Korea, Republic of |
Patent informations
| Patent description | Representative patent | Categories | Patent holder | Licence with MPP | Patent source |
|---|---|---|---|---|---|
|
Bedaquiline fumarate salt and solid compositions
Expiry date: 2027-12-03 Bedaquiline fumarate salt, pharmaceutical compositions comprising as active ingredient said salt and to processes for their preparation. |
WO2008068231 | Salt | Aelterman, Wim, Albert, Alex, Faure, Anne, Hegyi, Jean Francois, Alexandre, Lucas, Janssen Pharmaceutica N.V, Lang, Yolande, Lydia, Leys, Carina, Stokbroekx, Sigrid, Carl, Maria, Van Remoortere, Peter, Jozef, Maria | No |
Patent status
| Patent status/countries | Low, Low- middle and upper-middle | High income |
|---|---|---|
| Granted | Türkiye, Botswana, Gambia (the), Ghana, Kenya, Lesotho, Malawi, Mozambique, Namibia, Sierra Leone, Sudan, Eswatini, Tanzania, United Republic of, Uganda, Zambia, Zimbabwe, Turkmenistan, Belarus, Tajikistan, Kazakhstan, Azerbaijan, Kyrgyzstan, Armenia, Moldova, Republic of, Mexico, Peru, South Africa, Lebanon, Indonesia, Jordan, Montenegro, Philippines, Viet Nam, Kosovo, Sri Lanka, Benin, Cameroon, Burkina Faso, Chad, Guinea-Bissau, Mali, Senegal, Congo, Guinea, Gabon, Niger, Equatorial Guinea, Mauritania, Togo, Côte d'Ivoire, Central African Republic, Serbia, North Macedonia, Bosnia and Herzegovina, Albania | United States of America, Australia, Canada, Belgium, Germany, France, Luxembourg, Netherlands, Switzerland, United Kingdom, Sweden, Italy, Austria, Liechtenstein, Greece, Spain, Denmark, Monaco, Portugal, Ireland, Finland, Cyprus, Czechia, Estonia, Slovakia, Slovenia, Hungary, Romania, Poland, Iceland, Lithuania, Latvia, Malta, Japan, Korea, Republic of, Norway, New Zealand, Taiwan, Province of China, Chile, Russian Federation, Uruguay, Bahrain, Kuwait, Qatar, Saudi Arabia, Oman, United Arab Emirates, Israel, Brunei Darussalam, Panama, Singapore, Croatia |
| Filed | Venezuela (Bolivarian Republic of), Pakistan | |
| Not in force | Argentina, Brazil, China, Malaysia, India, World Intellectual Property Organization (WIPO), Ukraine, Thailand, Egypt | Bulgaria, Hong Kong, Japan, World Intellectual Property Organization (WIPO) |
Patent informations
| Patent description | Representative patent | Categories | Patent holder | Licence with MPP | Patent source |
|---|---|---|---|---|---|
|
Bedaquiline to treat latent TB
Expiry date: 2025-12-08 Use of bedaquiline for the manufacture of a medicament for the treatment of latent tuberculosis |
WO2006067048 | Use | Janssen Pharmaceutica N.V | No |
Patent status
| Patent status/countries | Low, Low- middle and upper-middle | High income |
|---|---|---|
| Granted | Jordan, Ukraine, Montenegro, Indonesia, Sri Lanka, Mexico, Pakistan | Canada, Australia, Bulgaria, Estonia, Latvia, Hong Kong, Croatia, Israel, Korea, Republic of, Norway, New Zealand, Taiwan, Province of China, Panama, Bahrain, Kuwait, Qatar, Saudi Arabia, Oman, United Arab Emirates, Macao, Malta, Singapore, Trinidad and Tobago |
| Filed | Nicaragua, Kosovo, Lebanon, Venezuela (Bolivarian Republic of) | Cyprus, Germany, Denmark, Spain, Portugal, Slovenia, Poland, Japan |
| Not in force | Türkiye, Argentina, Botswana, Gambia (the), Ghana, Kenya, Lesotho, Malawi, Mozambique, Namibia, Sierra Leone, Sudan, Eswatini, Tanzania, United Republic of, Uganda, Zambia, Zimbabwe, Brazil, China, Turkmenistan, Belarus, Tajikistan, Kazakhstan, Azerbaijan, Kyrgyzstan, Armenia, Moldova, Republic of, Malaysia, Serbia, South Africa, India, World Intellectual Property Organization (WIPO), Ecuador, Egypt, Benin, Cameroon, Burkina Faso, Chad, Guinea-Bissau, Mali, Senegal, Congo, Guinea, Gabon, Niger, Equatorial Guinea, Mauritania, Togo, Côte d'Ivoire, Central African Republic, Philippines, Thailand, Viet Nam, Albania, Bosnia and Herzegovina, North Macedonia | Bulgaria, Cyprus, Germany, Denmark, Belgium, France, Luxembourg, Netherlands, Switzerland, United Kingdom, Sweden, Italy, Austria, Liechtenstein, Greece, Spain, Monaco, Portugal, Ireland, Finland, Czechia, Estonia, Slovakia, Slovenia, Hungary, Romania, Poland, Iceland, Lithuania, Latvia, Croatia, Japan, Korea, Republic of, United States of America, Costa Rica, Russian Federation, World Intellectual Property Organization (WIPO) |
Patent informations
| Patent description | Representative patent | Categories | Patent holder | Licence with MPP | Patent source |
|---|---|---|---|---|---|
|
Bedaquiline to treat MDR TB and/or combinations with other antimycobacterial agents
Expiry date: 2025-05-24 The invention relates to the use of a substituted quinoline derivative for the preparation of a medicament for the treatment of an infection with a drug resistant Mycobacterium strain wherein the substituted quinoline derivative is a compound according to Formula (Ia) or Formula (Ib) the pharmaceutically acceptable acid or base addition salts thereof, the stereochemically isomeric forms thereof, the tautomeric forms thereof and the N-oxide forms thereof. Also claimed is a composition comprising a pharmaceutically acceptable carrier and, as active ingredient, a therapeutically effective amount of the above compounds and one or more other antimycobacterial agents. |
WO2005117875 | Use | Janssen Pharmaceutica N.V | No |
Patent status
| Patent status/countries | Low, Low- middle and upper-middle | High income |
|---|---|---|
| Granted | Mexico, Venezuela (Bolivarian Republic of), Viet Nam, Montenegro | Canada, Germany, Israel, Japan, Korea, Republic of, Norway, Russian Federation, Panama, Macao |
| Filed | Egypt | |
| Not in force | Türkiye, World Intellectual Property Organization (WIPO), Botswana, Gambia (the), Ghana, Kenya, Lesotho, Malawi, Mozambique, Namibia, Sierra Leone, Sudan, Eswatini, Tanzania, United Republic of, Uganda, Zambia, Zimbabwe, Argentina, Brazil, China, Turkmenistan, Belarus, Tajikistan, Kazakhstan, Azerbaijan, Kyrgyzstan, Armenia, Moldova, Republic of, Malaysia, Serbia, Ukraine, South Africa, India, Indonesia, Kosovo, Lebanon, Benin, Cameroon, Burkina Faso, Chad, Guinea-Bissau, Mali, Senegal, Congo, Guinea, Gabon, Niger, Equatorial Guinea, Mauritania, Togo, Côte d'Ivoire, Central African Republic, Pakistan, Philippines, Sri Lanka, Thailand, Jordan, Albania, Bosnia and Herzegovina, North Macedonia | Australia, Germany, Belgium, France, Luxembourg, Netherlands, Switzerland, United Kingdom, Sweden, Italy, Austria, Liechtenstein, Greece, Spain, Denmark, Monaco, Portugal, Ireland, Finland, Cyprus, Bulgaria, Czechia, Estonia, Slovakia, Slovenia, Hungary, Romania, Poland, Iceland, Lithuania, Hong Kong, Korea, Republic of, New Zealand, Taiwan, Province of China, United States of America, World Intellectual Property Organization (WIPO), Chile, Bahrain, Kuwait, Qatar, Saudi Arabia, Oman, United Arab Emirates, Croatia, Latvia |
Patent informations
| Patent description | Representative patent | Categories | Patent holder | Licence with MPP | Patent source |
|---|---|---|---|---|---|
|
Bedaquiline compounds
Expiry date: 2023-07-18 Novel compounds, in particular substituted quinoline derivatives, having the property of inhibiting growth of mycobacteria and therefore useful for the treatment of mycobacterial diseases, particularly those diseases caused by pathogenic mycobacteria such as Mycobacterium tuberculosis, M. bovis, M. avium and M. marinum. |
WO2004011436 | Compound | Janssen Pharmaceutica N.V | No |
Patent status
| Patent status/countries | Low, Low- middle and upper-middle | High income |
|---|---|---|
| Granted | Montenegro, Sri Lanka | United States of America, Belgium, Germany, France, Luxembourg, Netherlands, United Kingdom, Sweden, Italy, Austria, Greece, Denmark, Finland, Cyprus, Bulgaria, Estonia, Slovakia, Hungary, Romania, Russian Federation, Israel, Iceland, Japan, Korea, Republic of, Norway, Poland, Taiwan, Province of China, Chile, Latvia, Lithuania, Malta, Singapore |
| Filed | Cyprus | |
| Not in force | Türkiye, Argentina, Brazil, China, Turkmenistan, Belarus, Tajikistan, Kazakhstan, Azerbaijan, Kyrgyzstan, Armenia, Moldova, Republic of, World Intellectual Property Organization (WIPO), Mexico, Malaysia, Yugoslavia/Serbia and Montenegro, Ukraine, South Africa, India, Bosnia and Herzegovina, Egypt, Indonesia, Kosovo, Benin, Cameroon, Burkina Faso, Chad, Guinea-Bissau, Mali, Senegal, Congo, Guinea, Gabon, Niger, Equatorial Guinea, Mauritania, Togo, Côte d'Ivoire, Central African Republic, Pakistan, Philippines, Thailand, Viet Nam, Botswana, Gambia (the), Ghana, Kenya, Lesotho, Malawi, Mozambique, Sierra Leone, Sudan, Eswatini, Tanzania, United Republic of, Uganda, Zambia, Zimbabwe, Albania, North Macedonia | Australia, Canada, Belgium, Germany, France, Luxembourg, Netherlands, Switzerland, United Kingdom, Sweden, Italy, Austria, Liechtenstein, Greece, Spain, Denmark, Monaco, Portugal, Ireland, Finland, Cyprus, Bulgaria, Czechia, Estonia, Slovakia, Slovenia, Hungary, Romania, Hong Kong, Croatia, New Zealand, World Intellectual Property Organization (WIPO), Bahrain, Kuwait, Qatar, Saudi Arabia, Oman, United Arab Emirates, Latvia, Lithuania |
Supporting material
Publications
L. De Matteis, D. Jary, A. Lucía, S. García-Embid, I. Serrano-Sevilla, D. Pérez, J.A. Ainsa, F.P. Navarro, J. M. de la Fuente, New active formulations against M. tuberculosis: Bedaquiline encapsulation in lipid nanoparticles and chitosan nanocapsules, Chemical Engineering Journal, Volume 340, 2018, Pages 181-191, ISSN 1385-8947, https://doi.org/10.1016/j.cej.2017.12.110.
In the last years, the increase in antimicrobial resistance, together with a lack of new drugs for the treatment of bacterial infections resistant to classical antibiotics are of growing concern. Moreover, some of current therapies induce severe side effects and are often difficult to administer. In 2012 the FDA approved the use of bedaquiline, as the first new very effective drug against TB in the last 40 years. Despite its effectiveness, unfortunately bedaquiline side effects can be so dangerous that at present it is to be prescribed only when no other treatment options are available. The development of effective and safe nanotechnology-based methods can be particularly relevant to increase antimicrobial concentration at the site of infection, to reduce doses in the general circulation, which in turn reduces adverse effects. In this work bedaquiline was encapsulated in two types of nanocarriers, lipid nanoparticles and chitosan-based nanocapsules with high encapsulation efficiency and drug loading values. The efficacy of the drug-encapsulating nanocarriers has been demonstrated in vitro against Mycobacterium tuberculosis, together with the excellent compatibility of both carriers with animal cells. The obtained results open the way for further studies on multi-drug resistant strains of M. tuberculosis and for in vivo studies of the optimized nanocarriers. The promising behaviour of drug-loaded nanocarriers will hopefully lead to a reduction of the administered doses of a quite dangerous drug as bedaquiline, tuning its biodistribution and so decreasing its adverse effects, finally allowing its use in a higher number of patients.
Kaushik A, Ammerman NC, Tyagi S, Saini V, Vervoort I, Lachau-Durand S, Nuermberger E, Andries K. Activity of a Long-Acting Injectable Bedaquiline Formulation in a Paucibacillary Mouse Model of Latent Tuberculosis Infection. Antimicrob Agents Chemother. 2019 Mar 27;63(4):e00007-19. DOI: 10.1128/AAC.00007-19. PMID: 30745396; PMCID: PMC6437534.
The potent antituberculosis activity and long half-life of bedaquiline make it an attractive candidate for use in long-acting/extended-release formulations for the treatment of latent tuberculosis infection (LTBI). Our objective was to evaluate a long-acting injectable (LAI) bedaquiline formulation in a validated paucibacillary mouse model of LTBI. Following immunization with Mycobacterium bovis rBCG30, BALB/c mice were challenged by aerosol infection with M. tuberculosis H37Rv. Treatment began 13 weeks after challenge infection with one of the following regimens: an untreated negative-control regimen; positive-control regimens of daily rifampin (10 mg/kg of body weight), once-weekly rifapentine (15 mg/kg) and isoniazid (50 mg/kg), or daily bedaquiline (25 mg/kg); test regimens of one, two, or three monthly doses of LAI bedaquiline at 160 mg/dose (BLAI-160); and test regimens of daily bedaquiline at 2.67 mg/kg (B2.67), 5.33 mg/kg (B5.33), or 8 mg/kg (B8) to deliver the same total amount of bedaquiline as one, two, or three doses of BLAI-160, respectively. All drugs were administered orally, except for BLAI-160 (intramuscular injection). The primary outcome was the decline in M. tuberculosis lung CFU counts during 12 weeks of treatment. The negative- and positive-control regimens performed as expected. One, two, and three doses of BLAI-160 resulted in decreases of 2.9, 3.2, and 3.5 log10 CFU/lung, respectively, by week 12. Daily oral dosing with B2.67, B5.33, and B8 decreased lung CFU counts by 1.6, 2.8, and 4.1 log10, respectively. One dose of BLAI-160 exhibited activity for at least 12 weeks. The sustained activity of BLAI-160 indicates that it shows promise as a short-course LTBI treatment requiring few patient encounters to ensure treatment completion.
Van Hemelryck S, Wens R, van Poppel H, Luijks M, Shahidi K, Marczak M, Kahnt A, Holm R, Mannaert E, Langguth P. In Vitro Evaluation of Poly(lactide-co-glycolide) In Situ Forming Gels for Bedaquiline Fumarate Salt and Pharmacokinetics Following Subcutaneous Injection in Rats. Pharmaceutics. 2021 Aug 10;13(8):1231. DOI: 10.3390/pharmaceutics13081231. PMID: 34452192; PMCID: PMC8400137.
This study evaluated in vitro and in vivo drug release of bedaquiline from in situ forming gels (ISGs) containing 200 mg eq./g bedaquiline fumarate salt prepared with four different grades of poly(d,l-lactide) (PDLLA) or poly(d,l-lactide-co-glycolide) (PLGA) with a lactide/glycolide ratio of 50/50 or 75/25 and acid (A) or ester (E) end-capping in N-methyl-2-pyrrolidone at a polymer/solvent ratio of 20/80% (w/w). Mean in vitro drug release in 0.05 M phosphate buffer pH 7.4 with 1% (w/v) sodium lauryl sulphate was 37.3, 47.1, 53.3, and 62.3% within 28 days for ISGs containing PLGA5050A, PDLLA, PLGA7525A, and PLGA7525E, respectively. The data suggested that drug release was primarily controlled by precipitated drug redissolving, rather than polymer erosion. In vivo pharmacokinetic profiles after subcutaneous injections in rats were comparable for all ISGs (mean half-lives (t1/2) ranged from 1411 to 1695 h) and indicated a sustained drug release when compared to a solution of bedaquiline fumarate salt in polyethylene glycol 400/water 50/50% (v/v) (mean t1/2 of 895 h). In conclusion, PLGA or PDLLA-based ISGs have shown potential for parenteral sustained delivery of bedaquiline, suggesting further preclinical and clinical studies. From a formulation point of view, this case example highlights the importance of the interplay between drug solubility in biological media and dissolution of drug precipitates, which, in addition to the incorporation of diffusion controlling polymers, governs the release of the active drug.
Linking In Vitro Intrinsic Dissolution Rate and Thermodynamic Solubility with Pharmacokinetic Profiles of Bedaquiline Long-Acting Aqueous Microsuspensions in Rats. Vy Nguyen, Jan Bevernage, Nicolas Darville, Christophe Tistaert, Jan Van Bocxlaer, Stefaan Rossenu, and An Vermeulen. Molecular Pharmaceutics 2021 18 (3), 952-965. DOI: 10.1021/acs.molpharmaceut.0c00948
Pharmacokinetic (PK) profiles of a range of bedaquiline (BDQ) long-acting injectable (LAI) microsuspensions in rats after parenteral (i.e., intramuscular and subcutaneous) administration were correlated with the in vitro intrinsic dissolution rate (IDR) and thermodynamic solubility of BDQ in media varying in surfactant type and concentration to better understand the impact of different nonionic surfactants on the in vivo performance of BDQ LAI microsuspensions. All LAI formulations had a similar particle size distribution. The investigated surfactants were d-α-tocopheryl polyethylene glycol 1000 succinate (TPGS), poloxamer 338, and poloxamer 188. Furthermore, the relevance of medium complexity by using a biorelevant setup to perform in vitro measurements was assessed by comparing IDR and thermodynamic solubility results obtained in biorelevant media and formulation vehicle containing different surfactants in varying concentrations. In the presence of a surfactant, both media could be applied to obtain in vivo representative dissolution and solubility data because the difference between the biorelevant medium and formulation vehicle was predominantly nonsignificant. Therefore, a more simplistic medium in the presence of a surfactant was preferred to obtain in vitro measurements to predict the in vivo PK performance of LAI aqueous suspensions. The type of surfactant influenced the PK profiles of BDQ microsuspensions in rats, which could be the result of a surfactant effect on the IDR and/or thermodynamic solubility of BDQ. Overall, two surfactant groups could be differentiated: TPGS and poloxamers. Most differences between the PK profiles (i.e., maximum concentration observed, time of maximum concentration observed, and area under the curve) were observed during the first 21 days postdose, the time period during which particles in the aqueous suspension are expected to dissolve.
Kaushik A, Ammerman NC, Tasneen R, Lachau-Durand S, Andries K,Nuermberger E. Efficacy of long-acting bedaquiline regimens in a mouse model of tuberculosis preventive therapy. Am. J. Respir. Crit. Care Med. 2022;205:570–579. https://doi.org/10.1164/rccm.202012-4541OC.
Rationale: Completion of preventive therapy is a major bottleneck in global tuberculosis control. Long-acting injectable drug formulations would shorten therapy administration and may thereby improve completion rates. Recently, a long-acting formulation of bedaquiline demonstrated antituberculosis activity for up to 12 weeks after injection in a validated mouse model of preventive therapy.
Objectives: The objectives of this study were to 1) determine the total duration of activity after an injection of long-acting bedaquiline and 2) evaluate the activity of regimens comprised of long-acting bedaquiline plus short (2–4 wk) oral companion courses of bedaquiline, with or without rifapentine, using the validated mouse model of tuberculosis preventive therapy.
Methods: After the establishment of a stable Mycobacterium tuberculosis lung infection in bacillus Calmette-Guérin (BCG)-immunized BALB/c mice, treatment was initiated with 1 of 12 randomly assigned regimens. In addition to positive and negative controls, six regimens included one or two injections of long-acting bedaquiline (alone or with oral bedaquiline with or without rifapentine), and four comparator regimens consisted of oral agents only. Lung bacterial burden was measured monthly for up to 28 weeks.
Measurements and Main Results: One injection of long-acting bedaquiline at 160 mg/kg exerted antituberculosis activity for 12 weeks. Compared with the positive control (daily isoniazid-rifapentine for 4 wk), six regimens had equivalent bactericidal activity (including two all-oral comparator regimens), and two regimens had superior sterilizing activity: one injection with 2 weeks of oral bedaquiline and high-dose rifapentine; and two injections with 4 weeks of oral bedaquiline.
Conclusions: Long-acting injectable bedaquiline has significant potential for shortening tuberculosis preventive therapy.
Additional documents
No documents were uploaded
Useful links
There are no additional links
Access principles
|
|
Collaborate for developmentConsider on a case by case basis, collaborating on developing long acting products with potential significant public health impact, especially for low- and middle-income countries (LMICs), utilising the referred to long-acting technology Not provided |
|
|
Share technical information for match-making assessmentProvide necessary technical information to a potential partner, under confidentiality agreement, to enable preliminary assessment of whether specific medicines of public health importance in LMICs might be compatible with the referred to long-acting technology to achieve a public health benefit Not provided |
|
|
Work with MPP to expand access in LMICsIn the event that a product using the referred to long-acting technology is successfully developed, the technology IP holder(s) will work with the Medicines Patent Pool towards putting in place the most appropriate strategy for timely and affordable access in low and middle-income countries, including through licensing Not provided |
Comment & Information
Not provided