Drug information
Insulin icodec
Awiqli
Biotherapeutic
Insulin icodec is an ultra long-acting basal insulin analogue. It is a re-engineered version of the ultra long-acting oral basal insulin OI338, with several modifications introduced to significantly extend the half-life. These modifications - which cause increased serum albumin binding and attenuated insulin receptor affinity - result in a mean half-life of approximately 196 hours, allowing for once-weekly administration.
Insulin icodec was approved by Health Canada, EMA, Japan, Australia and Switzerland in 2024 for the treatment of adults living with type 1 or 2 diabetes mellitus. It has also been approved in Chine but only for the T2D indication. In July 2024, the US FDA rejected the approval of insulin icodec, citing concerns regarding manufacturing aspects and the indication being sought for type 1 diabetes.
AWIQLI 700 units/1 ml, 1500 units/1.5 ml, & 2100 units/3 mL is approved by several stringent regulatory authorities for management of type 2 diabetes mellitus (and for some, also type 1 diabetes).
Therapeutic area(s)
- Diabetes
- Treatment
Administration route
Subcutaneous
Associated long-acting platforms
Solution
Use of drug
- Administered by a community health worker
- Administered by a nurse
- Administered by a specialty health worker
- Self-administered
The reduced injection frequency of once-weekly insulin icodec has been linked to better adherence and acceptance among patients. Studies suggest that the lower injection burden could facilitate greater willingness to initiate or continue insulin therapy, particularly for individuals who find daily injections challenging. In ONWARDS2, T2DM patients using insulin icodec reported significantly higher satisfaction scores compared to those using daily basal insulins. In contrast, patient satisfaction was lower for insulin icodec compared to insulin degludec in type 1 diabetes (ONWARDS 6 trial).
Dosage
700 units/1mL; 1050 units/1.5mL & 2100 units/3mL
Once weekly
700 units per SC administration
For Type 1 Diabetes Mellitus—insulin icodec + bolus insulin combination therapy. For Type 2 Diabetes Mellitus —initial dose is 70 units, monotherapy, or combination therapy with sulfonylurea/GLP-1 agonist. For patients transitioning to Awiqli once-weekly insulin, both T1DM & T2DM—the recommended dose depends on their previous total daily dose of once- or twice-daily basal insulin. The dosage regimen is as follows: If the previous daily dose was 10 units, give 110 units of Awiqli in week 1 and 110 units in week 2. If the previous daily dose was 11 units, give 70 units of Awiqli in week 1 and 120 units in week 2. If the previous daily dose was 12 units, give 80 units of Awiqli in week 1 and 130 units in week 2. If the previous daily dose was 14 units, give 90 units of Awiqli in week 1.
The prefilled injection has a dose range of 10-700 units/injection (increase the dose by 10 units) No proprietary device is required to deliver insulin icodec. It is administered subcutaneously using a pre-filled pen injector, which is similar in design and technique to those used for other insulins. The pen contains a high-concentration formulation of 700 units/mL, ensuring that the injection volume remains comparable to once-daily basal insulin injections
Associated technologies
Not provided
Comment & Information
Developer(s)

Novo Nordisk is a global healthcare company specializing in diabetes care. Founded in Denmark in 1923, it is renowned for its leadership in insulin production and diabetes treatments. Novo Nordisk's product portfolio includes insulin analogs, GLP-1 receptor agonists, and other pharmaceuticals for managing diabetes and other chronic conditions.
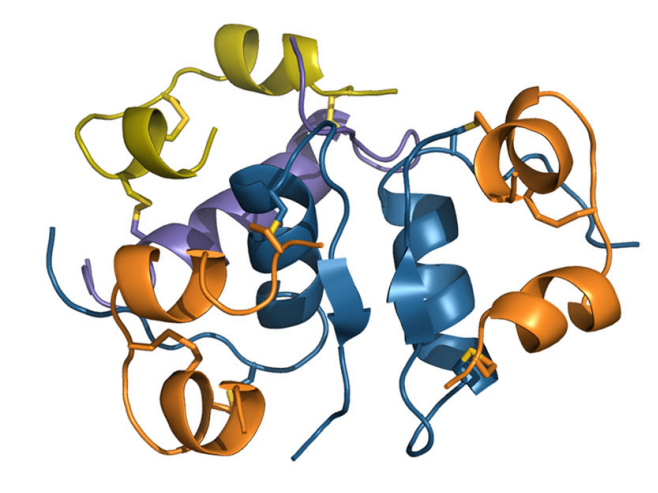
Drug structure
Scale-up and manufacturing prospects
In 2024, Novo Nordisk has invested 4.1 billion to expand the manufacturing capacity and increase the supply of AWQLI. It has five strategic production sites located in Denmark, the USA, France, Brazil, and China.
Peptide synthesizers, mixers, pH meters, and sterile filtration units. No proprietary device is required to deliver insulin icodec. It is administered subcutaneously using a pre-filled pen injector, which is similar in design and technique to those used for other insulins.
Manufacturing of Insulin icodec (Schedule D) follows ICH G7 guidelines. The manufacturing process includes: 1. Insulin icodec (Awiqli) is made using recombinant DNA technology in S. cerevisiae. 2. Drug substance steps: cell expansion, fermentation, recovery, concentration, and purification (incl. enzymatic/chemical steps). 3. Drug product: solution prep, mixing, pH/volume adjust, sterile filtration, aseptic fill into cartridges. 4. Final: capped, inspected, assembled, labelled, stored at 2–8°C. 5. Processes & controls are validated and acceptable.
1. High-Performance Liquid Chromatography (HPLC) 2. Mass Spectrometry (MS) and LC-MS (Liquid Chromatography-Mass Spectrometry) 3. Insulin Assay Kits or Immunoassays
Excipients
Not provided
Not provided
Not provided
Delivery device(s)
No delivery device
Icodec formulation
The invention provides a pharmaceutical composition comprising insulin icodec in a unique combination of excipients carefully formulated in order to reduce formation of oligomers at the injection site, while still showing PK/PD properties suited for a once-weekly administration. In another aspect, the invention provides a pharmaceutical composition with decreased viscosity upon injection and accordingly decreased propensity to create any discomfort upon injection. In another aspect, the invention provides a pharmaceutical composition with improved stability. In another aspect, the invention provides a pharmaceutical composition for use as a medicament for the treatment of a metabolic disorder.
WO2018109162
Composition
Novo Nordisk AS
Not provided
December 15, 2037
Granted in: CN, RU, ID, EP, VN, ZA, US; Filed in: BR, IN, PH, TH
Icodec formulation
A stable pharmaceutical formulation containing an insulin icodec that can conveniently be prepared by adding glycerol, phenol, m-cresol and zinc ions to it. Another aspect of this invention relates to the furnishing of insulin formulations having a relatively high content of insulin, e.g., a concentration of insulin above about 1 .5 mM insulin, preferably above about 3 mM insulin, and more preferred above about 4 mM and a concentration below about 9 mM insulin. Another aspect of this invention relates to the furnishing of insulin formulations having a sufficient chemical stability, a sufficient physical stability, a sufficiently low viscosity, a sufficient solubility and a sufficient stable oligomerisation pattern.
WO2013153000
Composition
Novo Nordisk AS
Not provided
April 5, 2033
Granted in CN, US, EP Filed in: RU Not in force: BR
Insulin Icodec compound and analogues
Novel acylated insulin analogues exhibiting resistance towards proteases can, effectively, be administered pulmonary or orally. The insulin analogues contain B25H and A14E or A14H.
WO2009115469
Compound
Novo Nordisk AS
Not provided
March 13, 2029
Granted: AU, BR, CN, IN, JP, MX, RU, ZA, EP, KR, US
Publications
Kjeldsen, T. B., Hubálek, F., Hjørringgaard, C. U., Tagmose, T. M., Nishimura, E., Stidsen, C. E., Porsgaard, T., Fledelius, C., Refsgaard, H. H. F., Gram-Nielsen, S., Naver, H., Pridal, L., Hoeg-Jensen, T., Jeppesen, C. B., Manfè, V., Ludvigsen, S., Lautrup-Larsen, I., & Madsen, P. (2021). Molecular Engineering of Insulin Icodec, the First Acylated Insulin Analog for Once-Weekly Administration in Humans. Journal of medicinal chemistry, 64(13), 8942–8950. https://doi.org/10.1021/acs.jmedchem.1c00257
Here, we describe the molecular engineering of insulin icodec to achieve a plasma half-life of 196 h in humans, suitable for once-weekly subcutaneously administration. Insulin icodec is based on re-engineering of the ultra-long oral basal insulin OI338 with a plasma half-life of 70 h in humans. This systematic re-engineering was accomplished by (1) further increasing the albumin binding by changing the fatty diacid from a 1,18-octadecanedioic acid (C18) to a 1,20-icosanedioic acid (C20) and (2) further reducing the insulin receptor affinity by the B16Tyr → His substitution. Insulin icodec was selected by screening for long intravenous plasma half-life in dogs while ensuring glucose-lowering potency following subcutaneous administration in rats. The ensuing structure-activity relationship resulted in insulin icodec. In phase-2 clinical trial, once-weekly insulin icodec provided safe and efficacious glycemic control comparable to once-daily insulin glargine in type 2 diabetes patients. The structure-activity relationship study leading to insulin icodec is presented here.
Hubálek, F., Cramer, C. N., Helleberg, H., Johansson, E., Nishimura, E., Schluckebier, G., Steensgaard, D. B., Sturis, J., & Kjeldsen, T. B. (2024). Enhanced disulphide bond stability contributes to the once-weekly profile of insulin icodec. Nature communications, 15(1), 6124. https://doi.org/10.1038/s41467-024-50477-9
Insulin icodec is a once-weekly insulin analogue that has a long half-life of approximately 7 days, making it suitable for once weekly dosing. The Insulin icodec molecule was developed based on the hypothesis that lowering insulin receptor affinity and introducing a strong albumin-binding moiety would result in a long insulin half-life, provided that non-receptor-mediated clearance is diminished. Here, we report an insulin clearance mechanism, resulting in the splitting of insulin molecules into its A-chain and B-chain by a thiol-disulphide exchange reaction. Even though the substitutions in insulin icodec significantly stabilise insulin against such degradation, some free B-chain is observed in plasma samples from minipigs and people with type 2 diabetes. In summary, we identify thiol-disulphide exchange reactions to be an important insulin clearance mechanism and find that stabilising insulin icodec towards this reaction significantly contributes to its long pharmacokinetic/pharmacodynamic profile.
Additional documents
Useful links
There are no additional links
Collaborate for development
Consider on a case by case basis, collaborating on developing long acting products with potential significant public health impact, especially for low- and middle-income countries (LMICs), utilising the referred to long-acting technology
Share technical information for match-making assessment
Provide necessary technical information to a potential partner, under confidentiality agreement, to enable preliminary assessment of whether specific medicines of public health importance in LMICs might be compatible with the referred to long-acting technology to achieve a public health benefit
Work with MPP to expand access in LMICs
In the event that a product using the referred to long-acting technology is successfully developed, the technology IP holder(s) will work with the Medicines Patent Pool towards putting in place the most appropriate strategy for timely and affordable access in low and middle-income countries, including through licensing