Drug information
Not provided
budigalimab
Not provided
Biotherapeutic
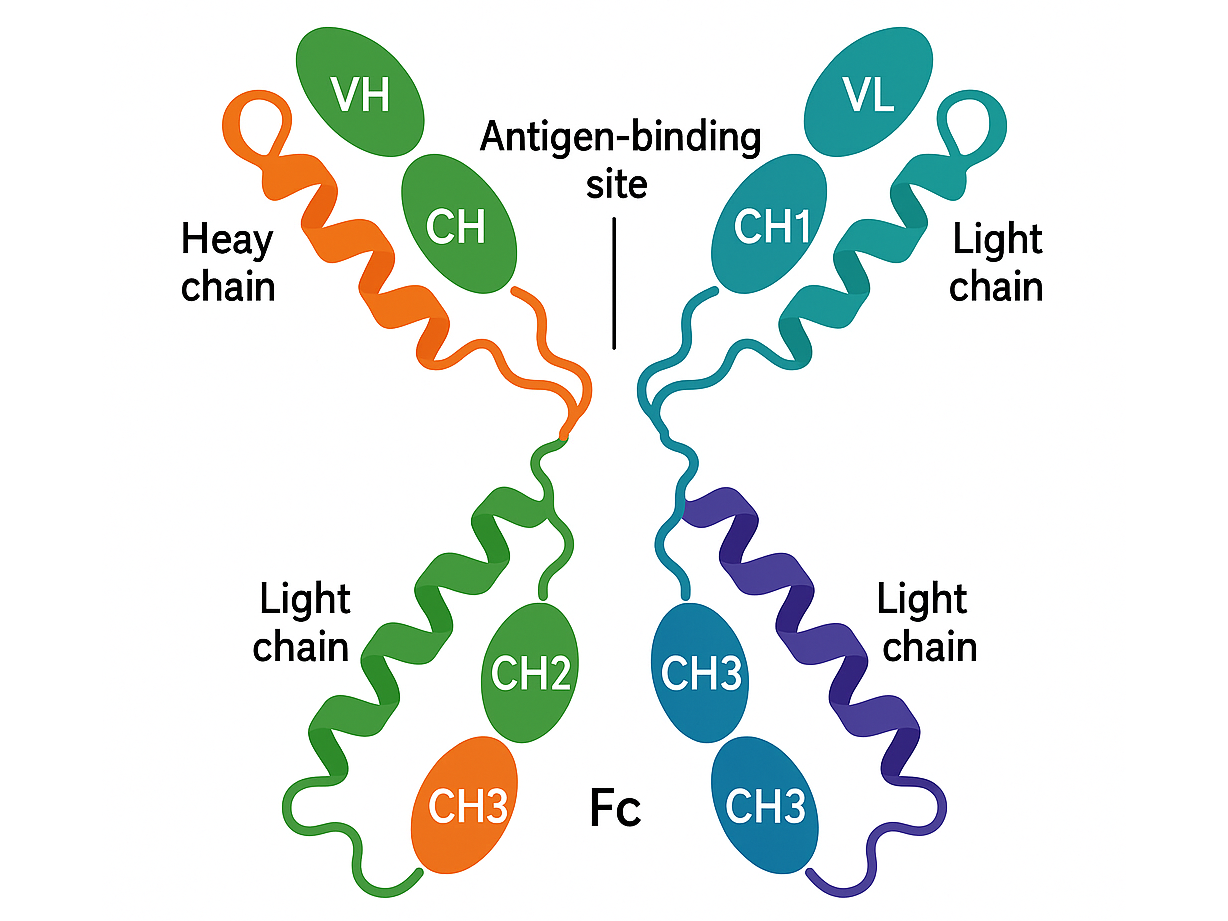
Budigalimab (ABBV-181) is an investigational anti-PD-1 monoclonal antibody developed for treating solid tumors and hematological malignancies. It binds to the PD-1 receptor on activated T cells, blocking interactions with its ligands, PD-L1 and PD-L2, thereby restoring T-cell activity and promoting anti-tumor immune responses. This mechanism is similar to that of approved checkpoint inhibitors like nivolumab and pembrolizumab. Budigalimab exhibits linear pharmacokinetics, with a half-life of approximately 14–17 days, clearance of 0.22–0.29 L/day, and a volume of distribution of 4–6 L. It reaches steady-state levels after repeated intravenous dosing. Studies show that it also delays HIV rebound or sustained low viral load in a majority of people who interrupted antiretroviral therapy (ART)
Not yet approved
Not approved by any regulatory authorities for
Therapeutic area(s)
- HIV
- Oncology
- Treatment
Administration route
Intravenous
Associated long-acting platforms
Solution
Use of drug
- Administered by a community health worker
- Administered by a nurse
- Administered by a specialty health worker
Not provided
Dosage
250mg and 500mg
Every 2 weeks; Every 4 weeks
Not available
Budigalimab 250 mg intravenously Q2W Budigalimab 500 mg intravenously Q4W
Not provided
Not provided
Associated technologies
Not provided
Comment & Information
Developer(s)

AbbVie Inc. is an American pharmaceutical company headquartered in North Chicago, Illinois. It is a global biopharmaceutical company known for its focus on developing treatments in several therapeutic areas, including immunology, oncology, neuroscience, and virology. It was founded in 2013 as a spin-off from Abbott Laboratories to focus specifically on pharmaceuticals.
Drug structure
Scale-up and manufacturing prospects
Not provided
Not provided
• Cell Line Development using CHO (Chinese Hamster Ovary) cell line. • Upstream Processing (USP): Cell Culture & Fermentation in bioreactors • Downstream Processing (DSP): Purification using Ion-Exchange Chromatography • Size exclusion chromatography (SEC) to remove aggregates and fragments
• SEC-HPLC, SDS-PAGE, Mass spectrometry, peptide mapping
Excipients
Not provided
Not provided
Not provided
Delivery device(s)
No delivery device
There are either no relevant patents or these were not yet submitted to LAPaL
Publications
Italiano, A., Cassier, P. A., Lin, C. C., Alanko, T., Peltola, K. J., Gazzah, A., Shiah, H. S., Calvo, E., Cervantes, A., Roda, D., Tosi, D., Gao, B., Millward, M., Warburton, L., Tanner, M., Englert, S., Lambert, S., Parikh, A., Afar, D. E., Vosganian, G., … Moreno, V. (2022). First-in-human phase 1 study of budigalimab, an anti-PD-1 inhibitor, in patients with non-small cell lung cancer and head and neck squamous cell carcinoma. Cancer immunology, immunotherapy : CII, 71(2), 417–431. https://doi.org/10.1007/s00262-021-02973-w
Abstract
Background: Budigalimab is a humanized, recombinant immunoglobulin G1 monoclonal antibody targeting programmed cell death protein 1 (PD-1). We present the safety, efficacy, pharmacokinetic (PK), and pharmacodynamic data from patients enrolled in the head and neck squamous cell carcinoma (HNSCC) and non-small cell lung cancer (NSCLC) expansion cohorts of the phase 1 first-in-human study of budigalimab monotherapy (NCT03000257; registered 15 December 2016).
Patients and methods: Patients with recurrent/metastatic HNSCC or locally advanced/metastatic NSCLC naive to PD-1/PD-1-ligand inhibitors were enrolled; patients were not selected on the basis of oncogene driver mutations or PD-L1 status. Budigalimab was administered at 250 mg intravenously Q2W or 500 mg intravenously Q4W until disease progression/unacceptable toxicity. The primary endpoints were safety and PK; the secondary endpoint was efficacy. Exploratory endpoints included biomarker assessments.
Results: In total, 81 patients were enrolled (HNSCC: N = 41 [PD-L1 positive: n = 19]; NSCLC: N = 40 [PD-L1 positive: n = 16]); median treatment duration was 72 days (range, 1-617) and 71 days (range, 1-490) for the HNSCC and NSCLC cohorts, respectively. The most frequent grade ≥ 3 treatment-emergent adverse event was anemia (HNSCC: n = 9, 22%; NSCLC: n = 5, 13%). Both dosing regimens had comparable drug exposure and increased interferon gamma-induced chemokines, monokine induced by gamma interferon, and interferon-gamma-inducible protein 10. Objective response rates were 13% (90% CI, 5.1-24.5) in the HNSCC cohort and 19% (90% CI, 9.2-32.6) in the NSCLC cohort. Median progression-free survival was 3.6 months (95% CI, 1.7-4.7) and 1.9 months (95% CI, 1.7-3.7) in the HNSCC and NSCLC cohorts.
Conclusions: The safety, efficacy and biomarker profiles of budigalimab are similar to other PD-1 inhibitors. Development of budigalimab in combination with novel anticancer agents is ongoing.
Calvo, E., Spira, A., Miguel, M., Kondo, S., Gazzah, A., Millward, M., Prenen, H., Rottey, S., Warburton, L., Alanko, T., Cassier, P. A., Yoh, K., Italiano, A., Moreno, V., Peltola, K., Seto, T., Toyozawa, R., Afar, D. E., Englert, S., Komarnitsky, P., … Gao, B. (2021). Safety, pharmacokinetics, and efficacy of budigalimab with rovalpituzumab tesirine in patients with small cell lung cancer. Cancer treatment and research communications, 28, 100405. https://doi.org/10.1016/j.ctarc.2021.100405
Abstract
Background: Agents targeting programmed cell death protein 1 (PD-1) have been approved as monotherapy for patients with small cell lung cancer (SCLC). In preclinical models, the combined targeting of PD-1 and delta-like protein 3 resulted in enhanced antitumor activity. Herein, we report results from the expansion arm of study NCT03000257 evaluating the combination of the anti-PD-1 antibody budigalimab and the targeted antibody-drug conjugate rovalpituzumab tesirine (Rova-T) in patients with previously treated SCLC.
Materials and methods: This expansion arm of a multicenter, open-label, multi-arm, first-in-human phase 1 clinical trial enrolled adult patients with progressive SCLC. The primary objective was to assess safety and tolerability. Patients received budigalimab 375 mg via intravenous infusion every 3 weeks, and Rova-T was administered as a dose of 0.3 mg/kg intravenously, on day 1 of the first and third 3-week cycle.
Results: As of October 2019, 31 patients with SCLC were enrolled and treated with budigalimab plus Rova-T. The combination was tolerated, with the most common treatment-emergent adverse events (in >30%) being pleural effusion, fatigue, and cough. The overall response rate was 24.1%, with one confirmed complete response and six confirmed partial responses. The overall response rate in patients with high delta-like protein 3 expression was similar (21.1%). The median progression-free survival was 3.48 months.
Conclusion: Combination therapy with budigalimab and Rova-T had promising efficacy and appeared to be tolerated in patients with SCLC. Although Rova-T development has been discontinued, development of budigalimab combined with other anticancer agents is ongoing.
Additional documents
No documents were uploaded
Useful links
There are no additional links
Collaborate for development
Consider on a case by case basis, collaborating on developing long acting products with potential significant public health impact, especially for low- and middle-income countries (LMICs), utilising the referred to long-acting technology
Share technical information for match-making assessment
Provide necessary technical information to a potential partner, under confidentiality agreement, to enable preliminary assessment of whether specific medicines of public health importance in LMICs might be compatible with the referred to long-acting technology to achieve a public health benefit
Work with MPP to expand access in LMICs
In the event that a product using the referred to long-acting technology is successfully developed, the technology IP holder(s) will work with the Medicines Patent Pool towards putting in place the most appropriate strategy for timely and affordable access in low and middle-income countries, including through licensing