Drug name
Cabotegravir + Rilpivirine
Drug information
Cabotegravir + Rilpivirine
Cabenuva (Cabotegravir and Rilpivirine co-packaged medication) and Vocabria (Cabotegravir) co-administered with Rekambys (Rilpivirine)
Small molecule
Long-acting injectable Cabotegravir and Rilpivirine (CAB/RPV-LA) is a complete treatment regimen for HIV-1 infection consisting of two components: (1) Cabotegravir a HIV-1 integrase strand transfer inhibitor developed by ViiV Healthcare and (2) Rilpivirine a second-generation non-nucleoside reverse transcriptase inhibitor manufactured by Janssen. CAB/RPV-LA is designated for the treatment of HIV-1 infection.
Cabotegravir and Rilpivirine extended-release injectable suspensions co-packaged as CABENUVA is approved by several Sringent Regulatory Authorities. Individually packaged extended-release Cabotegravir (VOCABRIA) and extended-release Rilpivirine (REKAMBYS) are approved for co-administration by various regulatory authorities for the treatment of HIV-1 infection. CAB+RPV LA injectables are awaiting approval in several countries.
CAB + RPV combination has received supplemental NDA approval with an Extended Label from the USFDA, inclusion in the Black Triangle Symbol Scheme by TGA Australia, and European Marketing Authorization by the EMA. This combination is specifically indicated for virologically suppressed adults with HIV-1 infection (HIV-1 RNA <50 copies per millilitre [c/ml]), weighing at least 35 kg. Eligible patients must have previously maintained stability on a treatment regimen without experiencing treatment failure or showing signs of resistance to Rilpivirine/Cabotegravir.
Therapeutic area(s)
- HIV
- Treatment
Administration route
Oral, Intramuscular
Associated long-acting platforms
Aqueous drug particle suspension
Use of drug
- Administered by a nurse
- Administered by a specialty health worker
- Self-administered
Not provided
Not provided
Dosage
Not provided
Not provided
Not provided
Not provided
Not provided
Associated technologies
Not provided
Comment & Information
Developer(s)

ViiV Healthcare is a pharmaceutical company that specializes in the development of therapies for HIV infection. The company is headquartered in Brentford in the United Kingdom and was initially formed in November 2009 as a part of a joint venture between GlaxoSmithKline and Pfizer.

Janssen Pharmaceuticals is a subsidiary company of Johnson & Johnson headquartered in Beerse, Belgium. They manufacture and develop pharmaceutical products for use in areas such as, Immunology, Infectious Diseases & Vaccines, Pulmonary Hypertension, Cardiovascular & Metabolism, Oncology, and Neuroscience.
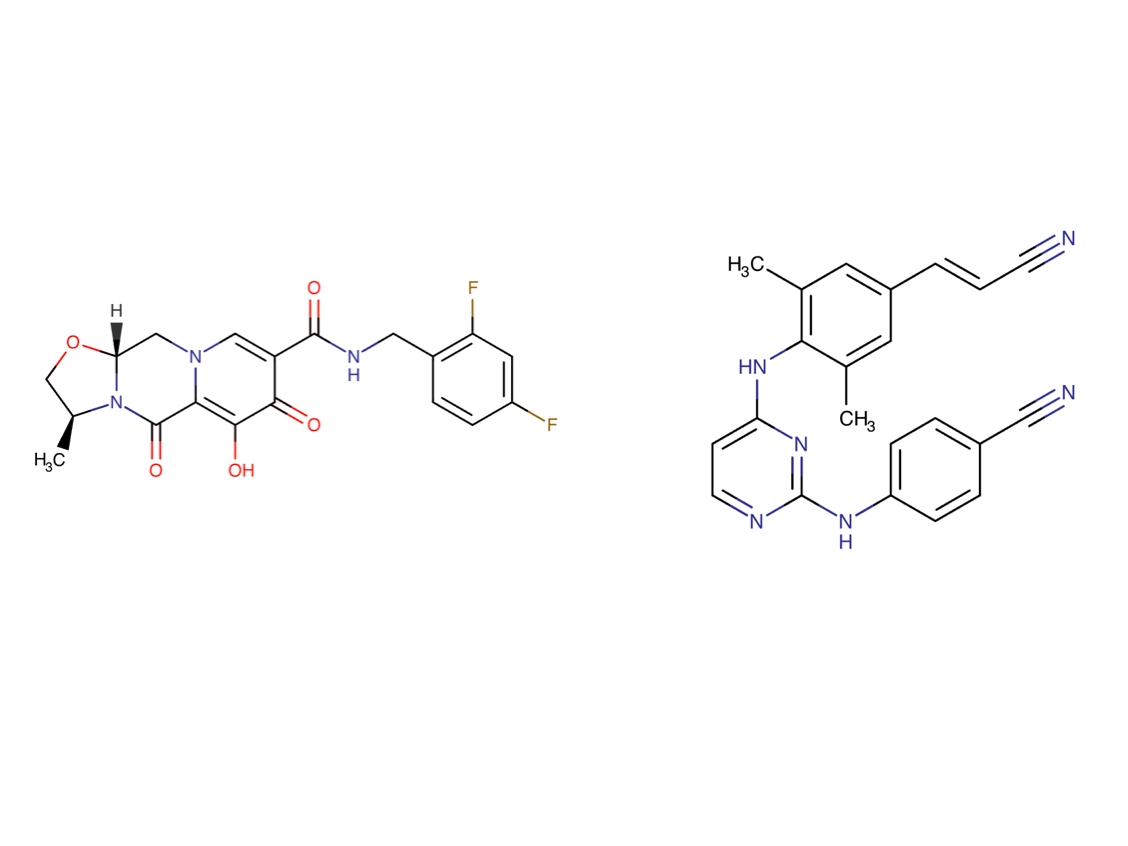
ViiV Healthcare(Vocabria) / Janssen-Cilag Ltd (Rekambys)Drug structure
Scale-up and manufacturing prospects
Compounds are commercially manufactured.
Conventional wet-bead milling apparatus (e.g. Netzsch ball mill), depyrogenated glass vials, high pressure homogenizer.
Cabotegravir and Rilpivirine are formulated into a wet-mill suspension of approximately 200mg/ml and 300mg/ml respectively, due to their low aqueous solubility. This formulation results in the creation of nanocrystal drug particles which are amenable for intramuscular gluteal depot injection. The manufacturing process for RPV is considered to be non-standard due to the inclusion of an aseptic processing step. RPV is light-sensitive, and exposure to light can induce conversion into a Z-isomer form which can affect pharmacokinetic data and activity.
PANalytical X’Pert PRO diffractometer equipped with a theta/theta coupled goniometer (or equivalent x-ray powder diffractor), Mettler TGA/DSC 1 instrument for thermal analysis, Laser diffractor (determine particle size), FT-IR UHPLC (chemical identification), UHPLC (chromatographic purity), paddle apparatus & UPLC/UV (determine in-vitro drug release for QC / dissolution testing).
Excipients
No proprietary excipient used
The novel excipient poloxamer 338 (P338) is used in the final G001 Rilpivirine clinical formulation. Following both an in-vitro mammalian chromosome aberration and an Ames test, it was considered to be non-genotoxic with no evidence for mutagenicity. Further P338 fertility, genotoxicity and development studies have been conducted with no negative effects, in addition to a 6-week and 9- month minipig repeat-dose toxicity study. No adverse local or systemic toxicity was reported in the minipigs at 100mg/month (Margin of Exposure:19).
No residual solvent used
Delivery device(s)
No delivery device
Publications
Bares SH, Scarsi KK. A new paradigm for antiretroviral delivery: long-acting cabotegravir and rilpivirine for the treatment and prevention of HIV. Curr Opin HIV AIDS. 2022 Jan 1;17(1):22-31. doi: https://doi.org/10.1097/COH.0000000000000708. PMID: 34871188; PMCID: PMC8694245.
Purpose of review
Cabotegravir (CAB) and rilpivirine (RPV) is the first long-acting injectable antiretroviral therapy (ART) option approved for virologically suppressed adults with HIV-1. In addition, long-acting CAB is a promising agent for HIV preexposure prophylaxis (PrEP). This review focuses on phase 3 clinical trial results and implementation considerations for these long-acting ART and PrEP strategies.
Recent findings
Long-acting CAB and RPV administered every 4 weeks demonstrated noninferiority to oral ART through week 96 in both the ATLAS and FLAIR studies, whereas ATLAS-2M found similar efficacy through 96 weeks when the long-acting injectable ART was administered every 8 weeks instead of every 4 weeks. For prevention, two phase 3 trials were stopped early due to fewer incident HIV infections in participants receiving long-acting CAB every 8 weeks compared with daily oral tenofovir disoproxil fumarate–emtricitabine for PrEP. The long-acting therapies were well tolerated across all clinical trials.
Summary
Clinical trial results support the use of long-acting CAB for HIV PrEP and long-acting CAB and RPV as a switch strategy for adults with HIV-1 who are first virologically suppressed with oral ART. Implementation challenges persist, and data are urgently needed in populations who may benefit most from long-acting therapy, including adolescents, pregnant individuals, and those with barriers to medication adherence.
Fostering implementation of health services research findings into practice: a consolidated framework for advancing implementation science. Damschroder LJ, Aron DC, Keith RE, Kirsh SR, Alexander JA, Lowery JC. Implement Sci. 2009;4:50. Published 2009 Aug 7. doi:10.1186/1748-5908-4-50
Background: Many interventions found to be effective in health services research studies fail to translate into meaningful patient care outcomes across multiple contexts. Health services researchers recognize the need to evaluate not only summative outcomes but also formative outcomes to assess the extent to which implementation is effective in a specific setting, prolongs sustainability, and promotes dissemination into other settings. Many implementation theories have been published to help promote effective implementation. However, they overlap considerably in the constructs included in individual theories, and a comparison of theories reveals that each is missing important constructs included in other theories. In addition, terminology and definitions are not consistent across theories. We describe the Consolidated Framework For Implementation Research (CFIR) that offers an overarching typology to promote implementation theory development and verification about what works where and why across multiple contexts.
Methods: We used a snowball sampling approach to identify published theories that were evaluated to identify constructs based on strength of conceptual or empirical support for influence on implementation, consistency in definitions, alignment with our own findings, and potential for measurement. We combined constructs across published theories that had different labels but were redundant or overlapping in definition, and we parsed apart constructs that conflated underlying concepts.
Results: The CFIR is composed of five major domains: intervention characteristics, outer setting, inner setting, characteristics of the individuals involved, and the process of implementation. Eight constructs were identified related to the intervention (e.g., evidence strength and quality), four constructs were identified related to outer setting (e.g., patient needs and resources), 12 constructs were identified related to inner setting (e.g., culture, leadership engagement), five constructs were identified related to individual characteristics, and eight constructs were identified related to process (e.g., plan, evaluate, and reflect). We present explicit definitions for each construct.
Conclusion: The CFIR provides a pragmatic structure for approaching complex, interacting, multi-level, and transient states of constructs in the real world by embracing, consolidating, and unifying key constructs from published implementation theories. It can be used to guide formative evaluations and build the implementation knowledge base across multiple studies and settings.
Outcomes for implementation research: conceptual distinctions, measurement challenges, and research agenda. Proctor E, Silmere H, Raghavan R, et al. Adm Policy Ment Health. 2011;38(2):65-76. doi:10.1007/s10488-010-0319-7
An unresolved issue in the field of implementation research is how to conceptualize and evaluate successful implementation. This paper advances the concept of "implementation outcomes" distinct from service system and clinical treatment outcomes. This paper proposes a heuristic, working "taxonomy" of eight conceptually distinct implementation outcomes-acceptability, adoption, appropriateness, feasibility, fidelity, implementation cost, penetration, and sustainability-along with their nominal definitions. We propose a two-pronged agenda for research on implementation outcomes. Conceptualizing and measuring implementation outcomes will advance understanding of implementation processes, enhance efficiency in implementation research, and pave the way for studies of the comparative effectiveness of implementation strategies.
Chloe Orkin, Rosalie Hayes, Joanne Haviland, Yuk Lam Wong, Kyle Ring, Vanessa Apea, Bakita Kasadha, Emily Clarke, Ruth Byrne, Julie Fox, Tristan J Barber, Amanda Clarke, Sara Paparini, For the ILANA study Group (Sadna Ullah, Nishat Halim, Chikondi Mwendera, James Hand), Perspectives of People With HIV on Implementing Long-acting Cabotegravir Plus Rilpivirine in Clinics and Community Settings in the United Kingdom: Results From the Antisexist, Antiracist, Antiageist Implementing Long-acting Novel Antiretrovirals Study, Clinical Infectious Diseases, Volume 80, Issue 5, 15 May 2025, Pages 1103–1113, https://doi.org/10.1093/cid/ciae523
Introduction
The equity-focused Implementing Long-Acting Novel Antiretrovirals study evaluated feasibility, acceptability, appropriateness of delivering on-label 2-monthly cabotegravir and rilpivirine (CAB + RPV) injections for human immunodeficiency virus (HIV)-1 therapy in clinics and community settings.
Methods
The study, which mandated inclusive recruitment, was conducted May–December 2022 at 6 UK sites. Injections were delivered in clinic (month [M] 1–6) and in clinic or community setting according to patient choice (M6–12). Surveys were completed at baseline, M4, and M12 using validated measures for feasibility (FIM), acceptability (AIM), and appropriateness (IAM). Primary endpoint: proportion of participants agreeing that the injection and community setting were feasible (FIM ≥4) at M12. Fourteen participants completed interviews at baseline and M12.
Results
Community settings offered by sites included: home visits (n = 3), HIV support organizations (n = 2), and community clinic (n = 1). Of 114 participants, 54% were female, 70% racially minoritized, and 40% aged ≥50 years. A total of 27/114 chose to receive injections in community settings. FIM/AIM/IAM scores at M12 were high for the injection (79.0–87.4%) and lower for the community setting (44.2–47.4%) overall. Subgroup analyses indicated differences in scores by gender and ethnicity. Among those who attended the community, FIM/AIM/IAM scores for the community setting at M12 were high (73.1–80.8%). Concerns about stigma, inconvenience, and losing access to trusted clinicians negatively influenced perceptions of receiving injections at community settings, amongst other factors.
Conclusions
CAB + RPV injections were considered highly feasible, acceptable, and appropriate; however, few chose community delivery. Those that chose community delivery found it highly acceptable and feasible. Further exploration of CAB + RPV delivery in alternative community sites not offered (eg, primary care, pharmacies) is warranted.
John M, Williams L, Nolan G, Bonnett M, Castley A, Nolan D. Real-world use of long-acting cabotegravir and rilpivirine: 12-month results of the inJectable Antiretroviral therapy feasiBility Study (JABS). HIV Med. 2024; 25(8): 935-945. doi:10.1111/hiv.13647
Objectives
The inJectable Antiretroviral feasiBility Study (JABS) aimed to evaluate the implementation of long-acting regimens in a ‘real world’ Australian setting, with inclusion of participants with complex medical needs, social vulnerability and/or historical non-adherence.
Methods
JABS was a 12-month, single-centre, single-arm, open-label phase IV study of long-acting cabotegravir 600 mg plus rilpivirine 900 mg administered intramuscularly every 2 months to adults with treated HIV-1 infection. The primary endpoint was the proportion of attendances and administration of injections within a 14-day dosing window over 12 months, out of the total prescribed doses. Secondary endpoints included proportions of missed appointments, use of oral bridging, discontinuations, virological failures, adverse events and participant-reported outcomes. A multidisciplinary adherence programme embedded in the clinical service known as REACH provided support to JABS participants.
Results
Of 60 participants enrolled by May 2022, 60% had one or more complexity or vulnerability factors identified, including absence of social supports (50%), mental health issues, alcohol or drug use (30%) and financial hardship or instability (13%), among others. Twenty-seven per cent of participants had historical non-adherence to antiretroviral therapy. Out of 395 prescribed doses, 97.2% of injections were administered within correct dosing windows at clinic visits. Two courses of short-term oral bridging were required. The rate of injection site reactions was 29%, the majority being grade 1–2. There were no virological failures, no serious adverse events and only one injection-related study discontinuation. High baseline treatment satisfaction and acceptability of injections increased by month 12. Those with vulnerability factors had similar adherence to injections as those without such factors. Ninety-eight per cent of the participants who completed 12 months on the study have maintained long-acting therapy, virological suppression and retention in care.
Conclusions
Long-acting cabotegravir plus rilpivirine was associated with very high adherence, maintenance of virological suppression, safety and treatment satisfaction in a diverse Australian clinic population, comparable to results of phase III randomized clinical trials. Individuals with vulnerability factors can achieve adherence to injections with individualized support. Long-acting therapies in this group can increase the subsequent engagement in clinical care.
Switch to long-acting cabotegravir and rilpivirine in virologically suppressed adults with HIV in Africa (CARES): week 48 results from a randomised, multicentre, open-label, non-inferiority trial. Kityo Cissy, Mugerwa Henry et al. The Lancet Infectious Diseases, Volume 24, Issue 10, 1083 - 1092
Background
Long-acting injectable cabotegravir and rilpivirine is licensed for individualised treatment of HIV-1 infection in resource-rich settings. Additional evidence is required to support use in African treatment programmes where demographic factors, viral subtypes, previous treatment, and delivery and monitoring approaches differ. The aim of this study was to determine whether switching to long-acting therapy with injections every 8 weeks is non-inferior to daily oral therapy in Africa.
Methods
CARES is a randomised, open-label, non-inferiority trial being conducted at eight sites in Uganda, Kenya, and South Africa. Participants with HIV viral load below 50 copies per mL on oral antiretroviral therapy and no history of virological failure were randomly assigned (1:1; web-based, permuted blocks) to receive cabotegravir (600 mg) and rilpivirine (900 mg) by intramuscular injection every 8 weeks, or to continue oral therapy. Viral load was monitored every 24 weeks. The primary outcome was week 48 viral load below 50 copies per mL, assessed with the Food and Drug Administration snapshot algorithm (non-inferiority margin 10 percentage points) in the intention-to-treat exposed population. This trial is registered with the Pan African Clinical Trials Registry (202104874490818) and is ongoing up to 96 weeks.
Findings
Between Sept 1, 2021, and Aug 31, 2022, we enrolled 512 participants (295 [58%] female; 380 [74%] previous non-nucleoside reverse transcriptase inhibitor exposure). Week 48 viral load was below 50 copies per mL in 246 (96%) of 255 participants in the long-acting therapy group and 250 (97%) of 257 in the oral therapy group (difference –0·8 percentage points; 95% CI –3·7 to 2·3), demonstrating non-inferiority (confirmed in per-protocol analysis). Two participants had virological failure in the long-acting therapy group, both with drug resistance; none had virological failure in the oral therapy group. Adverse events of grade 3 or greater severity occurred in 24 (9%) participants on long-acting therapy and ten (4%) on oral therapy; one participant discontinued long-acting therapy (for injection-site reaction).
Interpretation
Long-acting therapy had non-inferior efficacy compared with oral therapy, with a good safety profile, and can be considered for African treatment programmes.
Objectives:
Cabotegravir + rilpivirine (CAB + RPV) dosed monthly or every 2 months is the first complete long-acting (LA) regimen recommended by treatment guidelines for the maintenance of HIV-1 virological suppression. This post hoc analysis summarizes outcomes for Asian participants through week 96.
Methods:
Data from Asian participants naive to CAB + RPV randomized to receive dosing every 4 weeks (Q4W) or every 8 weeks (Q8W) in the FLAIR (NCT02938520) and ATLAS-2M (NCT03299049) phase 3/3b studies were pooled. The proportion of participants with plasma HIV-1 RNA ≥50 and <50 copies/mL (per FDA Snapshot algorithm), incidence of confirmed virological failure (CVF; two consecutive HIV-1 RNA ≥200 copies/mL), pharmacokinetics, safety, and tolerability through week 96 were assessed.
Results:
Overall, 41 Asian participants received CAB + RPV (Q8W, n = 17; Q4W, n = 24). At week 96, 83% (n = 34/41) of participants maintained HIV-1 RNA <50 copies/mL, none had HIV-1 RNA ≥50 copies/mL, and 17% (n = 7/41) had no virological data. No Asian participant met the CVF criterion. Drug-related adverse events occurred in 44% (n = 18/41) of participants; none were Grade ≥3. All injection site reactions were Grade 1 or 2; median duration was 2 days and most resolved within 7 days (90%, n = 390/435). CAB and RPV trough concentrations remained well above their respective proteinadjusted 90% inhibitory concentrations (CAB, 0.166 μg/mL; RPV, 12 ng/mL) through week 96.
Dima Dandachi, Cindy Garris, David Richardson, Gary Sinclair, Doug Cunningham, William Valenti, Bintu Sherif, Maria Reynolds, Kate Nelson, Deanna Merrill, Cathy Schubert, Kaitlin Nguyen, Ana Puga, Paula Teichner, Laurie Zografos, Clinical Outcomes and Perspectives of People With Human Immunodeficiency Virus Type 1 Twelve Months After Initiation of Long-acting Cabotegravir and Rilpivirine in an Observational Real-world US Study (BEYOND), Open Forum Infectious Diseases, Volume 12, Issue 5, May 2025, ofaf220, https://doi.org/10.1093/ofid/ofaf220
Background
Long-acting cabotegravir plus rilpivirine (CAB + RPV LA) administered monthly or every 2 months is recommended by treatment guidelines for maintenance of virologic suppression in people with human immunodeficiency virus type 1 (HIV-1). In clinical trials, CAB + RPV LA demonstrated noninferiority versus United States (US) Food and Drug Administration–approved daily oral therapy, and outcomes in real-world settings can supplement these results. We present month 12 results of BEYOND.
Methods
BEYOND is an ongoing, 2-year, multicenter, prospective, observational real-world study of adults initiating CAB + RPV LA in the US. Key outcomes included reasons for initiating, virologic outcomes, adherence, and patient-reported outcomes related to treatment satisfaction and treatment challenges at baseline and month 12.
Results
In total, 308 participants (median age, 45 years; 83% identified as male; 39% identified as Black) initiated CAB + RPV LA most commonly because of treatment fatigue, adherence anxiety with daily oral therapy, and/or convenience. Of participants with baseline viral load data, 97% (194/200) had a viral load <50 copies/mL for their most recent test reported at month 12. Mean treatment satisfaction scores increased significantly from baseline to month 12 and 97% (223/229) of participants preferred LA versus oral treatment at month 12. Proportions of participants reporting “always” or “often” experiencing challenges related to HIV-1 treatment (fear of disclosure, adherence anxiety, reminder of HIV-1 status, and feeling stigmatized) decreased from baseline to month 12.
Conclusions
Month 12 results from the real-world BEYOND study support the effectiveness of CAB + RPV LA for maintenance of virologic suppression and as a preferred treatment option for people with HIV-1.
Ford SL, Felizarta F, Han K, et al. Thigh Injections of Cabotegravir + Rilpivirine in Virally Suppressed Adults With Human Immunodeficiency Virus Type 1: A Substudy of the Phase 3b ATLAS-2M Study. Clin Infect Dis. Published online January 29, 2025. doi:10.1093/cid/ciae620
Background: Cabotegravir + rilpivirine (CAB + RPV) administered via intramuscular gluteal injections is the first complete long-acting regimen for maintaining human immunodeficiency virus type 1 (HIV-1) virologic suppression. We present substudy results on short-term repeat intramuscular CAB + RPV long-acting thigh injections in participants with ≥3 years of experience with gluteal administration during the ATLAS-2M study.
Methods: Substudy phases included screening, thigh injection (day 1-week 16), and return to gluteal injection (week 16-week 24). The injection schedule was unchanged from the main study. Outcomes included pharmacokinetics, safety, tolerability, efficacy, and patient-reported outcomes. Pharmacokinetic parameters were determined using noncompartmental analysis and mixed-effects modeling. Population pharmacokinetic simulations were performed.
Results: There were 118 participants. In the arm that received injections every 2 months (Q2M), first CAB thigh injection including area under the concentration-time curve and maximum observed concentration (Cmax) and first RPV thigh injection Cmax and all last RPV thigh injection parameters were statistically higher vs gluteal injections (paired comparison). No significant differences occurred with once-monthly (QM) dosing. No participants had HIV-1 RNA ≥50 copies/mL after thigh injections. Overall, 4%-7% of injection site reactions (ISRs) were grade 3. Five participants withdrew due to an ISR or injection intolerability. Overall, 30% preferred thigh vs gluteal injections. Simulations demonstrated the potential for chronic/continuous QM or ≤2 consecutive Q2M thigh injections.
Conclusions: These data demonstrate the potential use of chronic/continuous QM and rotational/short-term QM or Q2M (≤4 months of continuous dosing), CAB + RPV long-acting intramuscular thigh administration for HIV-1 treatment.
Additional documents
No documents were uploaded
Useful links
Collaborate for development
Consider on a case by case basis, collaborating on developing long acting products with potential significant public health impact, especially for low- and middle-income countries (LMICs), utilising the referred to long-acting technology
Share technical information for match-making assessment
Provide necessary technical information to a potential partner, under confidentiality agreement, to enable preliminary assessment of whether specific medicines of public health importance in LMICs might be compatible with the referred to long-acting technology to achieve a public health benefit
Work with MPP to expand access in LMICs
In the event that a product using the referred to long-acting technology is successfully developed, the technology IP holder(s) will work with the Medicines Patent Pool towards putting in place the most appropriate strategy for timely and affordable access in low and middle-income countries, including through licensing