Drug name
Lenacapavir (LEN)
Developer(s)
Drug information
Lenacapavir
Sunlenca
Small molecule
Capsid inhibitor
Lenacapavir (LEN), also known as GS-6207, is a first in-class HIV-1 capsid inhibitor used in combination with other antiretrovirals for the treatment of multi-drug resistant HIV-1 infection, and has potential application as HIV pre-exposure prophylaxis. LEN is utilised combinatorially for HIV-1 treatment, as it displays excellent synergy and no known cross-resistance with any other currently approved class of antiretroviral, in addition to possessing antiviral activity at picomolar levels.
For Treatment: Lenacapavir (SUNLENCA) 463.5mg/3ml subcutaneous injection with 300mg oral lead-in tablets are approved for use by 11 regualtory authorities (all for high income countries) for HIV-1 treatment under certain conditions. For PrEP: US FDA and South Africa has approved lenacapavir (Yeztugo) for HIV-1 prevention. It is also under review in Brazil, EU (+EEA), Australia, and Canada. Gilead has disclosed that it is preparing additional filings in countries that rely on FDA approval for regulatory submission, including Argentina, Mexico and Peru.
US FDA granted Breakthrough Therapy Designation for SUNLENCA in combination with other antiretroviral drugs for heavily treatment-experienced patients (HTE) adults with multi-drug resistant (MDR) HIV-1 infection failing their current antiretroviral regimen due to resistance, intolerance, or safety considerations. A European Marketing Authorization was issued for the use of SUNLENCA and it has also been classified as ‘Fast-Track Reimbursement’ by the Ministry of Health, Labour and Welfare, Japan, and ‘Part 1- Schedule 1 & Schedule 3 Poison’ by the Department of Health, Hong Kong. WHO guidelines released in July 2025 recommend offering six-monthly injectable lenacapavir as an additional PrEP option.
Therapeutic area(s)
- HIV
- Pre-Exposure Prophylaxis (PrEP)
- Treatment
- Prevention
Administration route
Oral, Subcutaneous, Intramuscular, To be determined
Associated long-acting platforms
Aqueous Solution, Oral solid form
Use of drug
- Administered by a community health worker
- Administered by a nurse
- Administered by a specialty health worker
- Self-administered
- To be determined
- Other/Variable/Unknown : Oral tablets 300 mg taken daily or weekly; Six-monthly injectable; Once-yearly investigational injectable.
Not provided
Dosage
LEN oral tablets 300 mg; each injection contains 927 mg of lenacapavir in solution. Dose for investigational Once-Yearly formulation is 5000 mg.
5000 mg
For PrEP: Initiation Option 1: Day 1: 927 mg by subcutaneous injection and 600 mg orally (2 x 300-mg tablets). Day 2: 600 mg orally (2 x 300-mg tablets). Initiation Option 2: Day 1: 600 mg orally (2 x 300-mg tablets). Day 2: 600 mg orally (2 x 300-mg tablets). Day 8: 300 mg orally (1 x 300-mg tablet). Day 15: 927 mg by subcutaneous injection. Maintenance: 927 mg by subcutaneous injection every 26 weeks +/- 2 weeks from date of last injection. For the treatment indication, lenacapavir is administered as part of a full treatment regimen with the relevant associated medicines.
Not provided
Not provided
Comment & Information
Developer(s)

Gilead Sciences Inc.
Gilead Sciences, Inc. is a multinational biopharmaceutical company that develops and manufactures innovative medicines for life-threatening diseases, including anti-viral therapeutics for HIV/AIDS, Hepatitis B, Hepatitis C and Covid-19. Headquartered in Foster City, California, Gilead was originally founded in 1987 and is currently listed on both the S&P 500 and the NASDAQ Biotechnology Index.
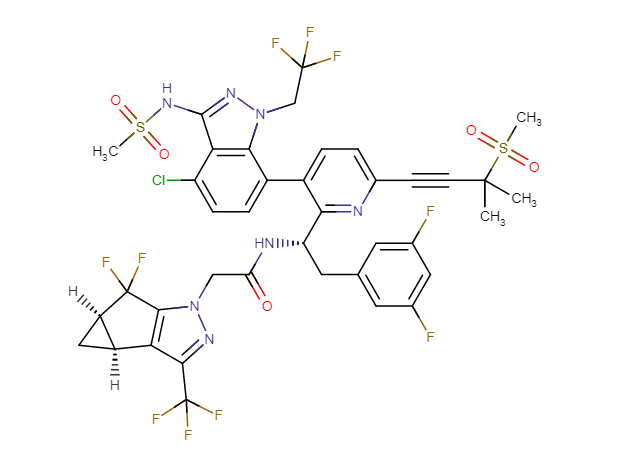
Drug structure
Scale-up and manufacturing prospects
Compound is commercially manufactured.
Equipment for injectable: Stainless steel pharmaceutical reactors, glass-lined reactors, rotary evaporator (rotovap), flash chromatography columns, stainless steel autoclave, cooling bath, silica gel chromatography columns, vacuum distillation apparatus, simulated moving bed chromatography system, Chiralpak columns.
Storage of injectable lenacapavir in borosilicate vials is contraindicated due to issues with chemical compatibility. Instead, it is recommended that vials are made from aluminosilicate glass.
Proton nuclear magnetic resonance (1H NMR), High-performance liquid chromatography (HPLC), Ultra-Performance Liquid Chromatography (UPLC).
Excipients
No proprietary excipient used
No novel excipient or existing excipient used
No residual solvent used
Delivery device(s)
No delivery device
Publications
Link JO, et al. Clinical targeting of HIV capsid protein with a long-acting small molecule. Nature. 2020 Aug;584(7822):614-618. doi: https://doi.org/10.1038/s41586-020-2443-1. Epub 2020 Jul 1.
Oral antiretroviral agents provide life-saving treatments for millions of people living with HIV, and can prevent new infections via pre-exposure prophylaxis1-5. However, some people living with HIV who are heavily treatment-experienced have limited or no treatment options, owing to multidrug resistance6. In addition, suboptimal adherence to oral daily regimens can negatively affect the outcome of treatment-which contributes to virologic failure, resistance generation and viral transmission-as well as of pre-exposure prophylaxis, leading to new infections1,2,4,7-9. Long-acting agents from new antiretroviral classes can provide much-needed treatment options for people living with HIV who are heavily treatment-experienced, and additionally can improve adherence10. Here we describe GS-6207, a small molecule that disrupts the functions of HIV capsid protein and is amenable to long-acting therapy owing to its high potency, low in vivo systemic clearance and slow release kinetics from the subcutaneous injection site. Drawing on X-ray crystallographic information, we designed GS-6207 to bind tightly at a conserved interface between capsid protein monomers, where it interferes with capsid-protein-mediated interactions between proteins that are essential for multiple phases of the viral replication cycle. GS-6207 exhibits antiviral activity at picomolar concentrations against all subtypes of HIV-1 that we tested, and shows high synergy and no cross-resistance with approved antiretroviral drugs. In phase-1 clinical studies, monotherapy with a single subcutaneous dose of GS-6207 (450 mg) resulted in a mean log10-transformed reduction of plasma viral load of 2.2 after 9 days, and showed sustained plasma exposure at antivirally active concentrations for more than 6 months. These results provide clinical validation for therapies that target the functions of HIV capsid protein, and demonstrate the potential of GS-6207 as a long-acting agent to treat or prevent infection with HIV.
Bester SM, Wei G, Zhao H, Adu-Ampratwum D, Iqbal N, Courouble VV, Francis AC, Annamalai AS, Singh PK, Shkriabai N, Van Blerkom P, Morrison J, Poeschla EM, Engelman AN, Melikyan GB, Griffin PR, Fuchs JR, Asturias FJ, Kvaratskhelia M: Structural and mechanistic bases for a potent HIV-1 capsid inhibitor. Science. 2020 Oct 16;370(6514):360-364. doi: https://doi.org/10.1126/science.abb4808
The potent HIV-1 capsid inhibitor GS-6207 is an investigational principal component of long-acting antiretroviral therapy. We found that GS-6207 inhibits HIV-1 by stabilizing and thereby preventing functional disassembly of the capsid shell in infected cells. X-ray crystallography, cryo-electron microscopy, and hydrogen-deuterium exchange experiments revealed that GS-6207 tightly binds two adjoining capsid subunits and promotes distal intra- and inter-hexamer interactions that stabilize the curved capsid lattice. In addition, GS-6207 interferes with capsid binding to the cellular HIV-1 cofactors Nup153 and CPSF6 that mediate viral nuclear import and direct integration into gene-rich regions of chromatin. These findings elucidate structural insights into the multimodal, potent antiviral activity of GS-6207 and provide a means for rationally developing second-generation therapies.
Marrazzo J. Lenacapavir for HIV-1 - Potential Promise of a Long-Acting Antiretroviral Drug. N Engl J Med. 2022;386(19):1848-1849. doi:10.1056/NEJMe2204376
As we walk through the lobby of a modern clinic for the treatment of patients with human immunodeficiency virus (HIV) infection or review antiretroviral regimens in the electronic medical record, it is easy to forget the days when managing multidrug-resistant HIV-1 was routine. Although the advent of protease inhibitors has saved lives,1 many patients already had resistance mutations to then-available nucleoside reverse-transcriptase inhibitors (NRTIs). For these patients and for others who contracted HIV infection with primary resistance, the subsequent iterative availability of new drug classes, including non-NRTIs and integrase-strand transferase inhibitors, essentially offered functional monotherapy against a background of complex resistance mutations. These patients continue to be among the most challenging to treat, even in well-resourced settings. At worst, treatment options may be exhausted; even if a suitable regimen can be designed, survival and quality of life are often compromised.2 Globally, among adults in whom non–NRTI-based first-line antiretroviral therapy has failed, 50 to 97% have evidence of resistance to these drugs.3
In this issue of the Journal, Segal-Maurer and colleagues4 describe a potentially new option for addressing this topic in the CAPELLA trial. Lenacapavir is a first-in-class capsid inhibitor with several important characteristics. First, it has two mechanisms of action at separate stages of the viral life cycle, thus posing a barrier to resistance that may be intrinsically higher. Second, it can be administered subcutaneously in infrequent injections up to every 6 months, which minimizes the pill burden and may improve adherence. Third, adverse events appear to be uncommon except for the formation of injection-site nodules or indurations in the small number of patients who have been evaluated. Finally, although resistance to lenacapavir was noted in 8 of 72 patients in the CAPELLA trial (mainly in those with M66I mutations), such resistance largely occurred early in the trial, and half these patients had poor adherence to their optimized background therapy. The early timing is reassuring because emergence of late resistance poses greater challenges to monitoring of the efficacy of antiretroviral therapy, especially in resource-limited settings. Moreover, some patients had viral suppression while continuing to receive lenacapavir, which suggests that reduced replication capacity of these mutants may translate into less fitness in maintaining infection.
Segal-Maurer et al. enrolled a highly treatment-experienced group of patients who had a median CD4+ count of 150 cells per cubic millimeter. The population notably included persons who are not always embraced in trials of new agents: adolescents (≥12 years of age) and patients with a relatively high body-mass index. The investigators used a rigorous definition of multidrug resistance and a two-cohort design that provided the opportunity to study lenacapavir in patients who were receiving different regimens. Cohort 1 included 36 patients who had stable viremia (i.e., a decrease of <0.5 log10 copies per milliliter between the screening and cohort-selection visits) and an HIV-1 RNA level of 400 copies or more per milliliter. These patients were randomly assigned in a 2:1 ratio to receive oral lenacapavir or matching placebo for the first 14 days, with the initiation of subcutaneous lenacapavir on day 15 and day 29, respectively. Cohort 2 included 36 patients (3 with reduced viremia and 33 who were enrolled after cohort 1 had been closed) who all received open-label oral lenacapavir with optimized background therapy on day 1 and started to receive subcutaneous lenacapavir once every 6 months on day 15. Follow-up occurred through week 52. Finally, the patients included an ethnically and racially diverse group that was representative of patients with HIV-1 infection — notably, 25% were women, 38% were Black, and 21% were Hispanic or Latinx. However, representation from Africa and Asia was limited.
The majority of patients in both cohorts had suppression of viremia, which was defined as a reduction of at least 0.5 log10 copies per milliliter in plasma HIV-1 RNA by day 15 (the primary efficacy end point measured at the end of the functional monotherapy period) and a viral load of less than 50 copies per milliliter and less than 200 copies per milliliter at week 26 after the initiation of subcutaneous lenacapavir. By day 15 in cohort 1, viral suppression had occurred in 88% of the patients in the lenacapavir group as compared with 17% of those in the placebo group. In cohort 2, the patients also had similar viral suppression, with a mean change from baseline in viral load of −2.49 log10 copies per milliliter by 26 weeks. Finally, lenacapavir treatment resulted in a least-squares mean increase from baseline in the CD4+ count of 75 cells per cubic millimeter in cohort 1 and 104 cells per cubic millimeter in cohort 2.
Although the number of patients in this trial was small, the CAPELLA trial offers support for HIV-1 treatment with long-acting agents with mechanisms of action that may minimize the development of resistance mutations. Equally exciting is the potential for the use of such agents as HIV-1 preexposure prophylaxis, for which lenacapavir is currently being evaluated. That said, several challenges remain — most notably, obstacles to establishing the safety and efficacy of very long-acting products in women of reproductive age (15 to 49 years) who are pregnant, are breast-feeding, or wish to become pregnant.5,6 The number of such women was projected to increase by 54% between 2015 and 2030 in sub-Saharan Africa, where the incidence of HIV-1 infection remains unacceptably high and access to modern contraceptives remains subpar.7 Nearly half of all infants born to women with HIV infection have resistance to one or more non-NRTIs.3 To truly change the trajectory of the global HIV pandemic, we must ensure expanded access to safe and effective life-changing medications for all patients.
Segal-Maurer S, DeJesus E, Stellbrink HJ, et al. Capsid Inhibition with Lenacapavir in Multidrug-Resistant HIV-1 Infection. N Engl J Med. 2022;386(19):1793-1803. doi:10.1056/NEJMoa2115542
Background:
Patients with multidrug-resistant human immunodeficiency virus type 1 (HIV-1) infection have limited treatment options. Lenacapavir is a first-in-class capsid inhibitor that showed substantial antiviral activity in a phase 1b study.
Methods:
In this phase 3 trial, we enrolled patients with multidrug-resistant HIV-1 infection in two cohorts, according to the change in the plasma HIV-1 RNA level between the screening and cohort-selection visits. In cohort 1, patients were first randomly assigned in a 2:1 ratio to receive oral lenacapavir or placebo in addition to their failing therapy for 14 days; during the maintenance period, starting on day 15, patients in the lenacapavir group received subcutaneous lenacapavir once every 6 months, and those in the placebo group received oral lenacapavir, followed by subcutaneous lenacapavir; both groups also received optimized background therapy. In cohort 2, all the patients received open-label oral lenacapavir with optimized background therapy on days 1 through 14; subcutaneous lenacapavir was then administered once every 6 months starting on day 15. The primary end point was the percentage of patients in cohort 1 who had a decrease of at least 0.5 log10 copies per milliliter in the viral load by day 15; a key secondary end point was a viral load of less than 50 copies per milliliter at week 26.
Results:
A total of 72 patients were enrolled, with 36 in each cohort. In cohort 1, a decrease of at least 0.5 log10 copies per milliliter in the viral load by day 15 was observed in 21 of 24 patients (88%) in the lenacapavir group and in 2 of 12 patients (17%) in the placebo group (absolute difference, 71 percentage points; 95% confidence interval, 35 to 90). At week 26, a viral load of less than 50 copies per milliliter was reported in 81% of the patients in cohort 1 and in 83% in cohort 2, with a least-squares mean increase in the CD4+ count of 75 and 104 cells per cubic millimeter, respectively. No serious adverse events related to lenacapavir were identified. In both cohorts, lenacapavir-related capsid substitutions that were associated with decreased susceptibility developed in 8 patients during the maintenance period (6 with M66I substitutions).
Conclusions:
In patients with multidrug-resistant HIV-1 infection, those who received lenacapavir had a greater reduction from baseline in viral load than those who received placebo. (Funded by Gilead Sciences; CAPELLA ClinicalTrials.gov number, NCT04150068.).
Łupina K, Nowak K, Lorek D, et al. Pharmacological advances in HIV treatment: from ART to long-acting injectable therapies. Arch Virol. 2025;170(9):195. Published 2025 Aug 19. doi:10.1007/s00705-025-06381-8
Human immunodeficiency virus (HIV) remains a global public health challenge, affecting millions worldwide despite significant advancements in antiretroviral therapy (ART). While ART has transformed HIV into a manageable chronic condition, long-term adherence, drug resistance, and access disparities continue to hinder treatment success. Recent research has focused on developing alternative therapeutic strategies, particularly long-acting injectable (LAI) therapies and immunotherapeutic approaches to improve adherence and potentially achieve viral remission. This review explores the evolution of pharmacological advancements in HIV treatment, highlighting the transition from daily oral ART to long-acting formulations such as cabotegravir, rilpivirine, and lenacapavir. LAI therapies reduce the burden of daily adherence, enhance treatment efficacy, and decrease stigma, particularly in vulnerable populations. Additionally, novel immunotherapeutic strategies such as broadly neutralizing antibodies, immune checkpoint inhibitors, and chimeric antigen receptor T cell therapy are being investigated for their potential to induce long-term viral suppression or cure. Despite these promising developments, several challenges remain, including resistance-associated mutations, accessibility issues, and long-term safety concerns. This review summarizes recent clinical trials, discusses the benefits and limitations of emerging HIV therapies, and outlines future research directions. The continued advancement of LAI therapies and immunotherapeutics holds great potential to improve treatment outcomes, expand global access to care, and move closer to a functional cure for HIV.
Saidi F, Hosseinipour MC, Chi BH. Long-Acting Injectable Antiretroviral Drugs for Pregnant and Breastfeeding Women: Current Advances, Challenges, and Future Directions. Curr HIV/AIDS Rep. 2025;22(1):44. Published 2025 Aug 15. doi:10.1007/s11904-025-00751-2
This review explores the promise and challenges of integrating long-acting antiretroviral agents-cabotegravir, lenacapavir, and cabotegravir-rilpivirine-into HIV prevention and treatment programs for pregnant and breastfeeding populations. It aims to examine current evidence, implementation experiences, and barriers to equitable access.
Emerging data support the efficacy and safety of long-acting agents during pregnancy and breastfeeding. Recent clinical trials have begun to include pregnant women by design, and national demonstration projects have successfully introduced injectable PrEP in maternal health settings. These developments signal growing recognition of the need for inclusive research and service delivery models. Long-acting antiretrovirals have the potential to transform maternal HIV prevention and treatment. However, challenges such as delayed inclusion in trials, policy constraints, limited product choice, high costs, and funding limitations persist. Addressing these gaps is critical to ensuring equitable access and informing future research and implementation strategies.
Pebody R. WHO recommends lenacapavir for HIV prevention. Lancet HIV. Published online August 5, 2025. doi:10.1016/S2352-3018(25)00224-3
WHO issued guidelines supporting the use of lenacapavir for pre-exposure prophylaxis (PrEP) on July 14, 2025, less than 13 months after the first press release announcing 100% efficacy in the PURPOSE-1 study.
Anderer S. WHO Recommends Lenacapavir for HIV Prevention in New Guidelines. JAMA. Published online August 1, 2025. doi:10.1001/jama.2025.10988
New guidelines released by the World Health Organization (WHO) recommend the use of injectable lenacapavir, the first twice-yearly preexposure prophylaxis (PrEP) option for HIV prevention.
The US Food and Drug Administration (FDA) recently approved the long-acting antiretroviral lenacapavir, marketed as Yeztugo, as an effective alternative to daily oral pills and other shorter-acting PrEP. Requiring only 2 doses per year, lenacapavir could be useful for people who face challenges with daily adherence, stigma, or access to health care, WHO noted.
The guidelines also state that rapid HIV diagnostic tests, which deliver results in less than 30 minutes, may be used to inform treatment decisions for long-acting PrEP. Assays of blood or saliva can reduce costs and minimize delays compared with nucleic acid testing techniques.
Access to lenacapavir remains limited in clinical settings, but WHO urges governments, donors, and global health partners to begin using the drug to diversify HIV prevention efforts as the infection continues to spread. In 2024, an estimated 1.3 million people were newly diagnosed with HIV, with a disproportionate risk among men who have sex with men, people who inject drugs, people in prisons, sex workers, and transgender individuals.
Kirby T. New lenacapavir guidelines from WHO. Lancet Infect Dis. Published online August 4, 2025. doi:10.1016/S1473-3099(25)00490-6
WHO has announced that twice-yearly injections of lenacapavir should be included as an additional HIV prevention option and that rapid diagnostic tests (RDTs) can be used for HIV testing for initiation, continuation, and discontinuation of lenacapavir and other long-acting and daily-oral pre-exposure prophylaxis (PrEP).
Lynch S, Cohen RM, Kavanagh M, et al. Lessons for long-acting lenacapavir: catalysing equitable PrEP access in low-income and middle-income countries. Lancet HIV. Published online July 11, 2025. doi:10.1016/S2352-3018(25)00161-4
Despite substantial advances in biomedical HIV prevention, including long-acting injectable pre-exposure prophylaxis (PrEP) options such as cabotegravir, barriers to widespread adoption and scale-up persist in low-income and middle-income countries. Long-acting injectable lenacapavir is a potentially transformative HIV prevention tool, providing an unprecedented opportunity to accelerate progress. However, the global HIV response is under threat like never before, with drastic funding cuts undermining the gains of the past 25 years. The challenges of introducing and scaling up long-acting lenacapavir and other PrEP innovations are numerous. Without deliberate policy, programmatic, and financing interventions, new prevention technologies risk following slow adoption patterns of previous innovations, weakening a needed transformation of the HIV response. Drawing on lessons from the scale-up of antiretroviral therapy, and experience with previous biomedical prevention tools, a new ten-point framework should be adopted to accelerate individual and epidemiological impact-even at this time of extraordinary uncertainty.
Vail RM, Cantor A, Shah SS, et al. Interim Guideline on the Use of Twice-Yearly Lenacapavir for HIV Prevention. Baltimore (MD): Johns Hopkins University; July 2025.
Subcutaneous Lenacapavir as PrEP
- Clinicians should recommend SC LEN as a preferred PrEP regimen for protection against HIV through sexual exposure for individuals who are willing to receive subcutaneous injections every 6 months and have no contraindications or barriers to its use. For other preferred PrEP regimens, see the NYSDOH AI guideline PrEP to Prevent HIV and Promote Sexual Health.
- Clinicians should discuss potential risks and benefits and engage individuals who are or may become pregnant in shared decision-making when considering SC LEN as PrEP.
Cantos VD, Ramírez BC, Kelley CF, Rio CD, Grinsztejn B. Lenacapavir: a potential game changer for HIV prevention in the Americas, if the game is played equitably. Lancet Reg Health Am. 2025;47:101146. Published 2025 Jun 10. doi:10.1016/j.lana.2025.101146
Lenacapavir, a first in class long-acting capsid inhibitor has near 100% efficacy in preventing HIV. As such, it has the potential to curb the rising HIV incidence in Latin America, a region with stark intra- and inter-country PrEP uptake disparities. In this viewpoint, we summarize the current efforts to scale up lenacapavir access globally and the necessary steps to include Latin America in these endeavours.
van Zyl G, Prochazka M, Schmidt HA, et al. Lenacapavir-associated drug resistance: implications for scaling up long-acting HIV pre-exposure prophylaxis. Lancet HIV. Published online June 18, 2025. doi:10.1016/S2352-3018(25)00128-6
Although drug resistance could emerge if lenacapavir is initiated during undiagnosed acute infection or if infection occurs during the drug's pharmacokinetic tail, these cases will not compromise the effectiveness of WHO-recommended therapies, as there is no cross-resistance between lenacapavir and other licensed antiretroviral drugs. Lenacapavir pre-exposure prophylaxis (PrEP) is also unlikely to drive population-level lenacapavir resistance given the rarity of breakthrough infections and the reduced replication capacity of most lenacapavir-resistant variants, which most likely reduces their transmission potential. Conversely, the risk of acquiring lenacapavir-resistant HIV-1 while receiving lenacapavir PrEP is likely to remain extremely low, as lenacapavir-associated drug-resistance mutations are rare among individuals without previous lenacapavir exposure, and widespread use of lenacapavir-based regimens remains years away. Nonetheless, as the number of lenacapavir PrEP programmes increase, surveillance for emerging lenacapavir resistance should also be implemented.
Additional documents
No documents were uploaded
Useful links
Collaborate for development
Consider on a case by case basis, collaborating on developing long acting products with potential significant public health impact, especially for low- and middle-income countries (LMICs), utilising the referred to long-acting technology
Share technical information for match-making assessment
Provide necessary technical information to a potential partner, under confidentiality agreement, to enable preliminary assessment of whether specific medicines of public health importance in LMICs might be compatible with the referred to long-acting technology to achieve a public health benefit
Work with MPP to expand access in LMICs
In the event that a product using the referred to long-acting technology is successfully developed, the technology IP holder(s) will work with the Medicines Patent Pool towards putting in place the most appropriate strategy for timely and affordable access in low and middle-income countries, including through licensing