Technology name
Vaginal Film (MATRIX)
Sponsor(s)
Type of technology
Vaginal film
Administration route
Topical (Vaginal)
Development state and regulatory approval
Dapivirine (DPV)
Phase I
Not provided
Description
Matrix vaginal film technology represents a novel, once-monthly, self-administered biodegradable polymer designed for the prevention of HIV and unplanned pregnancies. This polymer is typically cellulosic, such as carboxycellulose. Upon insertion into the vagina, contact with vaginal fluids initiates the slow dissolution of the film, facilitating the gradual release of API drug molecules. This delivery system ensures the sustained release of the API over the course of a month until complete dissolution of the film occurs and the entire drug is delivered locally.
Developer(s)

University of Pittsburgh
The University of Pittsburgh, founded in 1787, is one of the oldest universities in the United States. It has a notable research profile, particularly in biomedical research, engineering advancements, and public health initiatives. As a member of the prestigious Association of American Universities (AAU), it reflects a high level of research activity.

Magee-Womens Research Institute & Foundation
The Magee-Womens Research Institute (MWRI) is a renowned institution dedicated to advancing women's health through research and education. It specializes in areas such as reproductive biology, obstetrics, gynaecology, and women's cancers. MWRI has initiated numerous research studies aimed at improving healthcare outcomes for women globally, with a strong focus on personalized medicine.
Technology highlight
i. Made up of biodegradable polymer materials ii. Self-administration iii. Minimal impact on the innate microbiome iv. Low systemic toxicity
Illustration(s)
Technology main components
(i) HEC: HMC: CMC [or] HEC: HPMC: NaCMC (at varying concentrations) (ii) Plasticizer (eg: glycerin, polyethylene gylcol monomethyl ether, propylene glycol, sorbitol sorbitan solution, castor oil) (iii) Dispersant (iv) Humectant (v) Disintegrant (eg: PEG 400, PEG 6000; PEG 8000) (v) Solubilizing/ alkalizing agent (eg: sodium hydroxide)
Not provided
Delivery device(s)
Not provided
APIs compatibility profile
Antiretroviral drugs, including dapivirine, tenofovir disoproxil, and hormone replacement drugs such as levonorgestrel, are the focus of targeted drug of choice. Other targeted therapeutic classes include antibacterial, antiprotozoal, and antifungal drugs.
Not provided
Not provided
Not provided
2 different APIs : A combination of antiretroviral API and a hormonal API is been used.
Not provided
Scale-up and manufacturing prospects
Not provided
1) Elcometer 4340 Motorised/Automatic Film Applicator, Mixing vessels (with vacuum applicator) 2) Metrohm, 758 KFD Titrino 3) Coating and drying vessels 4) Packaging instrumentations (not specified)
The manufacturing of vaginal films using a Hot Melt Extrusion Process requires a cleanroom environment and involves several key steps: Feeding: Selected materials are introduced into an extruder. Melting: In the extruder, materials are heated to a temperature where polymers melt—above their melting point but below their decomposition temperature. Mixing: The molten material is mixed thoroughly to ensure even distribution of the API and excipients. Extrusion: The uniform mixture is extruded through a die to form a continuous sheet or film. Cooling: Extruded film is cooled rapidly to solidifies.
1) X-ray diffraction (To examine solid state solubility) 2) TX-XT Plus texture analyser 3) UPLC
Excipients
No proprietary excipient used
No novel excipient or existing excipient used
No residual solvent used
Additional features
- Biodegradable
- Drug-eluting
- Non-removable
- Reservoir-type
- Room temperature storage
Preclinical data indicate sufficient dissolution and drug release properties for a range of antiretroviral agents within the film matrix. Notably, a single-dose study of a 40 mg tenofovir (TFV) film demonstrated superior TFV delivery compared to the TFV vaginal gel formulation. Plasma and cervicovaginal fluid TFV concentrations were elevated on day 1 following TFV film administration compared to the gel, though levels converged by days 3 and 7 days later.
Not applicable
A Phase 1 clinical trial involving 78 healthy volunteers demonstrated that 91% of participants experienced solely Grade 1 adverse events (AEs). These AEs were evenly distributed across both the film tenofovir treatment and film placebo control groups, indicating a favourable safety and tolerability profile for the film formulation. Nevertheless, adherence challenges were reported by 50% of the study population.
A six-month accelerated stability test was conducted at 40°C to evaluate the integrity of vaginal films produced via hot melt extrusion. The results demonstrated that the weight of the films remained stable over the testing period. Variability in water content and puncture strength was found to be insignificant, indicating robust physical properties. The films with tenofovir showed good compatibility with various strains of lactobacilli as well.
Preclinical stability studies demonstrated no loss of API from vaginal films stored at 30, 40, and 50°C for 14 days. However, further investigation of storage conditions is warranted to establish long-term stability at cold storage conditions.
Therapeutic area(s)
- Contraception
- HIV
- Pre-Exposure Prophylaxis (PrEP)
Potential associated API(s)
- Dapivirine (DPV)
- Levonorgestrel (LNG)
Use of technology
- Self-administered
Monthly
Not provided
Targeted user groups
- Adults
- Older Adults
- Female
- Cisgender female
- Transgender female
No
Unspecified
Unspecified
Not provided
Antiretroviral agent
Phase I
NCT06046053
HIV
Not provided
Once monthly
Not provided
Levonorgestrel (LNG)
Synthetic progestin
Phase I
Not provided
Contraception and HIV prevention
18-50 years women
Once monthly
Not provided
Vaginal Films
Provided herein are stable, dissolvable films containing active ingredients, such as antimicrobial composition, antiviral compositions, or anti-retroviral compositions for intravaginal or intrarectal placement to provide prophylaxis against viral infections.
US20240099986A1
Device
University of Pittsburgh
Not provided
September 13, 2043
Granted
Hot melt extrusion for pharmaceutical vaginal film products
Hot melt extrusion is disclosed as a process for forming vaginal drug delivery films. The methods involve extruding a composition comprising one or more active pharmaceutical ingredients and one or more polymer carriers at an elevated temperature through a die to thereby provide the film. Films prepared by hot melt extrusion are also described.
US20230346693A1
Manufacturing Process
University of Pittsburgh
Not provided
May 3, 2043
Granted
Publications
Bunge, K. E., Dezzutti, C. S., Hendrix, C. W., Marzinke, M. A., Spiegel, H. M. L., Moncla, B. J., Schwartz, J. L., Meyn, L. A., Richardson-Harman, N., Rohan, L. C., & Hillier, S. L. (2018). FAME-04: A Phase 1 trial to assess the safety, acceptability, pharmacokinetics and pharmacodynamics of film and gel formulations of tenofovir. Journal of the International AIDS Society, 21(8), e25156. https://doi.org/10.1002/jia2.25156
Introduction: Fast-dissolving vaginal film formulations release antiretroviral drugs directly into vaginal fluid and may be as efficient at drug delivery yet more acceptable to women than gels. In this Phase 1 vaginal film study, the safety, acceptability, pharmacokinetics and pharmacodynamics of two doses of tenofovir (TFV) film and TFV 1% gel were compared to corresponding placebo formulations.
Methods: Seventy-eight healthy HIV negative women were randomized to self-insert daily vaginal film (10 mg TFV, 40 mg TFV or placebo) or 4 mL of vaginal gel (TFV 1% [40 mg] or placebo) for seven days. Grade 2 and higher adverse events (AEs) related to study product were compared across study arms using Fisher's exact test. Plasma TFV concentrations were measured before and 2 hours after last product use. Paired cervical and vaginal tissue biopsies obtained 2 hours after the last dose were measured to determine tenofovir diphosphate (TFV-DP) concentrations and exposed to HIV in an ex vivo challenge assay. Acceptability was assessed through questionnaire.
Results: There was only one grade 2 or higher related AE, the primary endpoint; it occurred in the placebo gel arm. AEs occurred in 90% of participants; the majority (91%) were grade 1. AEs were similar across study arms. TFV concentrations in plasma and TFV-DP concentrations in cervical and vaginal tissues were comparable between 40 mg TFV film and the TFV gel groups. There was a significant relationship between reduced viral replication and TFV-DP concentrations in cervical tissues. Film users were less likely to report product leakage than gel users (66% vs. 100%, p < 0.001).
Conclusions: Films were safe and well tolerated. Furthermore, films delivered TFV to mucosal tissues at concentrations similar to gel and were sufficient to block HIV infection of genital tissue ex vivo.
Fan, M. D., Kramzer, L. F., Hillier, S. L., Chang, J. C., Meyn, L. A., & Rohan, L. C. (2017). Preferred Physical Characteristics of Vaginal Film Microbicides for HIV Prevention in Pittsburgh Women. Archives of sexual behavior, 46(4), 1111–1119. https://doi.org/10.1007/s10508-016-0816-1
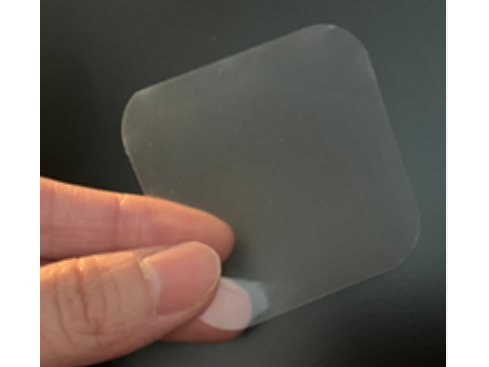
Unprotected heterosexual intercourse is the leading cause of HIV acquisition in women. Due to the complex nature of correct and consistent condom use by both men and women, developing alternative female-controlled HIV prevention options is a global health priority. Vaginal films containing antiretroviral drugs are a potential delivery system for the prevention of HIV acquisition through sexual contact. In this study, we explored women's preferences regarding physical characteristics of microbicide vaginal films through questionnaires and focus groups. Eighty-four sexually active, ethnically diverse women 18-30 years of age from Pittsburgh, Pennsylvania, participated in the study. Women visually and manually examined a variety of vaginal films, as well as three other vaginal products undergoing evaluation for HIV prevention: tablet, ring, and gel. Means and standard deviations or frequencies and 95 % confidence intervals were calculated for questionnaire data. Focus groups were audio-recorded, transcribed verbatim, and coded for content analysis. Women most frequently preferred vaginal films to be smooth and thin (63 %), translucent (48 %), and 2″ × 2″ square size (36 %). Driving these preferences were five major themes: ease and accuracy of use, desire for efficacy, discretion, intravaginal comfort and minimal impact, and minimizing disruption of sexual mood/activities. Women's preferences for various microbicide vaginal film physical attributes represented a balance of multiple values. In general, women desired a comfortable, efficacious, easy to use, and minimally intrusive product.
Robinson JA, Marzinke MA, Fuchs EJ, Bakshi RP, Spiegel HML, Coleman JS, Rohan LC, Hendrix CW. Comparison of the Pharmacokinetics and Pharmacodynamics of Single-Dose Tenofovir Vaginal Film and Gel Formulation (FAME 05). J Acquir Immune Defic Syndr. 2018 Feb 1;77(2):175-182. doi: 10.1097/QAI.0000000000001587. PMID: 29135651; PMCID: PMC5821271.
While pre-exposure prophylaxis with oral tenofovir (TFV) disoproxil fumarate/emtricitabine reduces HIV acquisition rates, poor adherence to and acceptability of daily vaginal gels has led to development of vaginal film formulations to improve adherence and, potentially, enable episodic use
In this two-arm, cross-over study of a fast-dissolving tenofovir film (40 mg) compared to a previously studied semisolid tenofovir 1% gel (40 mg), 10 healthy women received a single vaginal dose of each study product. Clinical, pharmacokinetic, and antiviral assessments were performed over one week post-dose. Nine of 10 participants experienced mild to moderate adverse effects, similar between products, with no severe adverse events or events attributed to study products. TFV concentrations after film dosing exceeded concentrations after gel dosing in plasma between 8 and 24 hours (p≤0.02). TFV concentrations in cervicovaginal fluid and both TFV and TFV diphosphate concentrations in cervical tissue homogenates were higher following film dosing (all p values < 0.04). The differences ranged from median (interquartile range) 2.9-fold (1.1, 9.0; midvaginal cervicovaginal fluid) to 4.4-fold (2.9, 7.7; plasma). Neither film nor gel demonstrated reduced cervical tissue biopsy infectivity after ex vivo HIV challenge. Single dose tenofovir film demonstrated consistently higher concentrations in plasma and cervicovaginal samples when compared to gel during the first day following dosing. Single dose cervical tissue TFV-DP concentrations at 5 hours exceeded steady-state concentrations previously reported with daily oral Truvada® dosing. Tenofovir film may provide an alternative to tenofovir oral and gel formulations. Clinical efficacy remains to be tested.
Additional documents
No documents were uploaded
Useful links
There are no additional links
Collaborate for development
Consider on a case by case basis, collaborating on developing long acting products with potential significant public health impact, especially for low- and middle-income countries (LMICs), utilising the referred to long-acting technology
Share technical information for match-making assessment
Provide necessary technical information to a potential partner, under confidentiality agreement, to enable preliminary assessment of whether specific medicines of public health importance in LMICs might be compatible with the referred to long-acting technology to achieve a public health benefit
Work with MPP to expand access in LMICs
In the event that a product using the referred to long-acting technology is successfully developed, the technology IP holder(s) will work with the Medicines Patent Pool towards putting in place the most appropriate strategy for timely and affordable access in low and middle-income countries, including through licensing








