Drug information
Cabotegravir and Lenacapavir
Apretude (CAB), Vocabria (CAB), Sunlenca (LEN)
Small molecule
Cabotegravir and Lenacapavir (CAB/LEN) is an investigational drug combination in clinical development for the treatment of HIV-1. Currently, the only approved complete long-acting ART therapy regimen in both the U.S. and Europe is a combination of intramuscular CAB and rilpivirine (CAB/RPV). This regimen is approved for individuals with prior viral suppression on oral ART. LEN is a novel HIV-1 capsid inhibitor administered via subcutaneous injection every 26 weeks and has recently been approved for the treatment of multidrug-resistant (MDR) HIV. While it has been studied in both treatment-naïve (CALIBRATE study) and MDR individuals (CAPELLA), the use of LEN in combination with CAB LA for individuals with NNRTI resistance and/or oral ART adherence challenges is currently being evaluated.
Given the limited number of available LA-ART medications, healthcare providers are increasingly prescribing injectable LEN through insurance programs and using it off-label with LA CAB (+/- RPV) for select patients with adherence challenges and NNRTI resistance.
Unknown
Therapeutic area(s)
- HIV
- Treatment
Administration route
Subcutaneous, Intramuscular
Associated long-acting platforms
Aqueous drug particle suspension, Aqueous solution
Use of drug
- Administered by a community health worker
- Administered by a nurse
Not provided
Dosage
Not provided
Not provided
Not provided
Not provided
Not provided
Not provided
Formulations
Compare
Cabotegravir and Lenacapavir
Lenacapavir Once-Yearly
MK-8591D (Islatravir and Lenacapavir)
Teropavimab and Zinlirvimab
Associated technologies
Not provided
Comment & Information
Developer(s)

ViiV Healthcare is a pharmaceutical company that specializes in the development of therapies for HIV infection. The company is headquartered in Brentford in the United Kingdom and was initially formed in November 2009 as a part of a joint venture between GlaxoSmithKline and Pfizer.

Gilead Sciences, Inc. is a multinational biopharmaceutical company that develops and manufactures innovative medicines for life-threatening diseases, including anti-viral therapeutics for HIV/AIDS, Hepatitis B, Hepatitis C and Covid-19. Headquartered in Foster City, California, Gilead was originally founded in 1987 and is currently listed on both the S&P 500 and the NASDAQ Biotechnology Index.
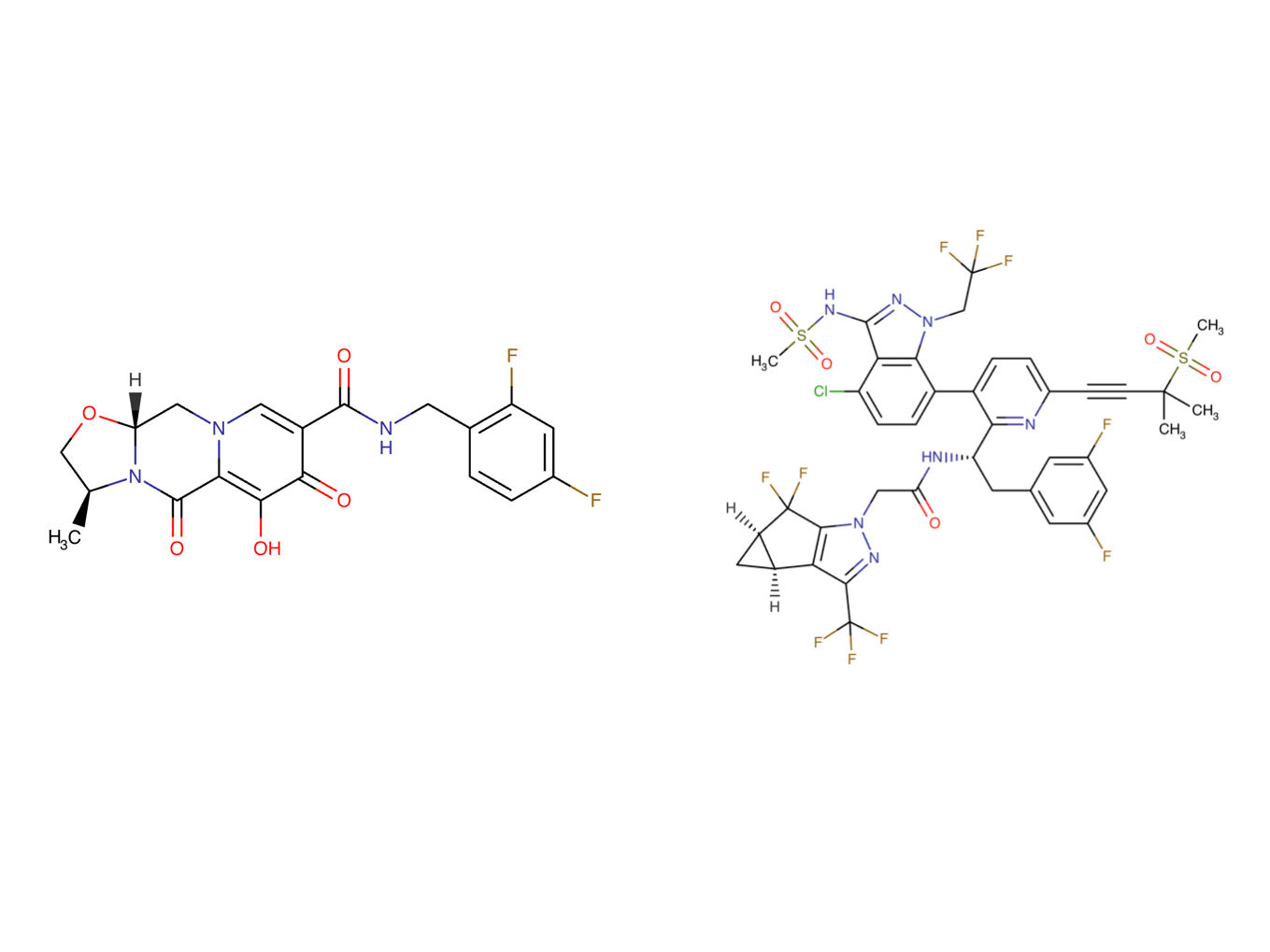
Drug structure
Scale-up and manufacturing prospects
Cabotegravir is commercially manufactured by the innovator (ViiV Healthcare) and three generic manufacturers have received a licence through the Medicines Patent Pool to manufacture generic versions by 2026/2027. Lenacapavir is commercially manufactured by Gilead Sciences Inc.
Cabotegravir: Conventional wet-bead milling (ball mill), depyrogenated glass vials. Lenacapavir: Equipment: Stainless steel pharmaceutical reactors, glass-lined reactors, rotary evaporator (rotovap), flash chromatography columns, stainless steel autoclave, cooling bath, silica gel chromatography columns, vacuum distillation apparatus, simulated moving bed chromatography system, Chiralpak columns.
Cabotegravir is subject to a gamma-irradiation pre-sterilization step prior to a conventional wet-bead milling manufacturing procedure. The Cabotegravir milling process is initiated alongside pharmaceutical excipients (polyethylene glycol 3350, water for injection, polysorbate 20 and mannitol) for an overall 200nm drug particle size. Storage of injectable lenacapavir in borosilicate vials is contraindicated due to issues with chemical compatibility. Instead, it is recommended that vials are made from aluminosilicate glass.
Cabotegravir: PANalytical X’Pert PRO diffractometer equipped with a theta/theta coupled goniometer (or equivalent x-ray powder diffractor) to determine drug particle size, Mettler TGA/DSC 1 instrument for thermal analysis, HPLC to evaluate drug content, impurities and dissolution, HPLC UV-Vis Detector for drug identification. Lenacapavir: Proton nuclear magnetic resonance (1H NMR), High-performance liquid chromatography (HPLC), Ultra-Performance Liquid Chromatography (UPLC).
Excipients
No proprietary excipient used
No novel excipient or existing excipient used
No residual solvent used
Delivery device(s)
No delivery device
There are either no relevant patents or these were not yet submitted to LAPaL
Publications
Gandhi M, Hill L, Grochowski J, Nelson A, Koss CA, Mayorga-Munoz F, Oskarsson J, Shiels M, Avery A, Bamford L, Baron J, Short WR, Hileman CO. Case Series of People With HIV on the Long-Acting Combination of Lenacapavir and Cabotegravir: Call for a Trial. Open Forum Infect Dis. 2024 Apr 16;11(4):ofae125. DOI: 10.1093/ofid/ofae125. PMID: 38628952; PMCID: PMC11020301.
Background
Injectable cabotegravir (CAB)/rilpivirine (RPV) is the only combination long-acting (LA) antiretroviral regimen approved for HIV. RPV may not be effective among individuals with non-nucleoside reverse transcriptase inhibitor (NNRTI) resistance, which has >10% prevalence in many countries. Lenacapavir (LEN) is an LA capsid inhibitor given every 6 months, but has not been studied in combination with other LA agents.
Methods
We assembled a case series from 4 US academic medical centers where patients with adherence challenges were prescribed LEN subcutaneously every 26 weeks/CAB (+/− RPV) intramuscularly every 4 or 8 weeks. Descriptive statistics, including viral load (VL) outcomes, were summarized.
Results
All patients (n = 34: 76% male; 24% cis/trans female; 41% Black; 38% Latino/a; median age [range], 47 [28–75] years; 29% and 71% on CAB every 4 or 8 weeks) reported challenges adhering to oral ART. The reasons for using LEN/CAB with or without RPV were documented or suspected NNRTI mutations (n = 21, 59%), integrase mutations (n = 5, 15%), high VL (n = 6, 18%), or continued viremia on CAB/RPV alone (n = 4, 12%). Injection site reactions on LA LEN were reported in 44% (32% grade I, 12% grade 2). All patients but 2 (32/34; 94%) were suppressed (VL <75 copies/mL) after starting LEN at a median (range) of 8 (4–16) weeks, with 16/34 (47%) suppressed at baseline.
Conclusions
In this case series of 34 patients on LEN/CAB, high rates of virologic suppression (94%) were observed. Reasons for using LEN/CAB included adherence challenges and underlying resistance, mostly to NNRTIs. These data support a clinical trial of LEN/CAB among persons with NNRTI resistance.
Additional documents
No documents were uploaded
Useful links
There are no additional links
Collaborate for development
Consider on a case by case basis, collaborating on developing long acting products with potential significant public health impact, especially for low- and middle-income countries (LMICs), utilising the referred to long-acting technology
Share technical information for match-making assessment
Provide necessary technical information to a potential partner, under confidentiality agreement, to enable preliminary assessment of whether specific medicines of public health importance in LMICs might be compatible with the referred to long-acting technology to achieve a public health benefit
Work with MPP to expand access in LMICs
In the event that a product using the referred to long-acting technology is successfully developed, the technology IP holder(s) will work with the Medicines Patent Pool towards putting in place the most appropriate strategy for timely and affordable access in low and middle-income countries, including through licensing