Drug information
Not provided
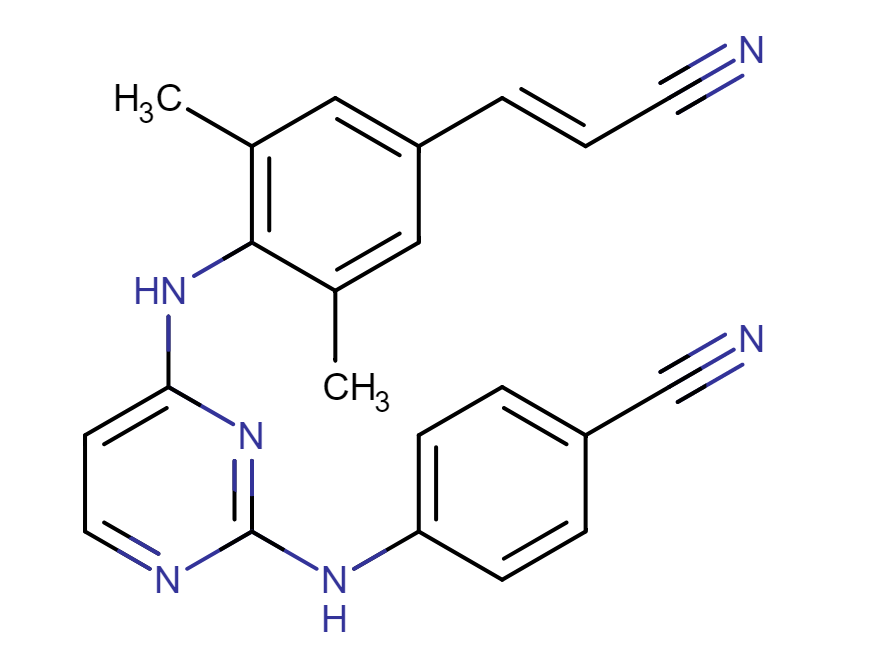
Rilpivirine
Edurant, Rekambys, Eviplera/Complera, Odefsey
Not provided
Rilpivirine (RPV), also known as TMC278, is a HIV-1 non-nucleoside reverse transcriptase inhibitor (NNRTI) used to treat antiretroviral naïve individuals with HIV. RPV is a derivative of diarylpyrimidine and functions by mechanistically binding to the HIV reverse transcriptase enzyme. This interaction prevents the conversion of RNA into viral DNA, which is an essential step in HIV infection. RPV is available in multiple formulations, including short-acting oral medication (Edurant) and combination tablets (Odefsey, Juluca and Eviplera/Complera), in addition to a long-acting intramuscular injectable (Rekambys). In Jan 2021, Rekambys received U.S. FDA approval to be administered alongside Vocabria (Cabotegravir) for HIV treatment in adults and adolescents weighing 77 pounds (35kg) or more.
Unknown
Unknown
Therapeutic area(s)
- HIV
- Pre-Exposure Prophylaxis (PrEP)
- Treatment
Administration route
Oral, Intramuscular
Associated long-acting platforms
Aqueous drug particle suspension
Use of drug
- Administered by a nurse
- Administered by a specialty health worker
Not provided
Dosage
Not provided
Not provided
Not provided
Not provided
Not provided
Not provided
Formulations
Compare
Rilpivirine Prodrug Nanoformulation (NM3RPV)
Associated technologies
Dissolving microarray patchesTunable Biodegradable Ultra-Long-Acting Polymeric Solid Implant (PSI)
LYNX
Thin Film Polycaprolactone Device Implant
ProTide Prodrug Technology
Comment & Information
Developer(s)

Janssen Pharmaceuticals is a subsidiary company of Johnson & Johnson headquartered in Beerse, Belgium. They manufacture and develop pharmaceutical products for use in areas such as, Immunology, Infectious Diseases & Vaccines, Pulmonary Hypertension, Cardiovascular & Metabolism, Oncology, and Neuroscience.
Drug structure
Scale-up and manufacturing prospects
Compound is commercially manufactured.
Netzsch ball mill, high pressure homogenizer.
The manufacturing process for RPV is considered to be non-standard due to the inclusion of an aseptic processing step. RPV is light-sensitive, and exposure to light can induce conversion into a Z-isomer form which can affect pharmacokinetic data and activity. Therefore, all processing, manufacturing and storage stages must implement mitigation procedures and protection from light. The RPV nanosuspension is stored aseptically in single-use glass vials with a protective nitrogen atmosphere. The formulation requires refrigerated storage and is stable for up to three years at 5°C.
Laser diffractor (determine particle size), FT-IR UHPLC (chemical identification), UHPLC (chromatographic purity), paddle apparatus & UPLC/UV (determine in-vitro drug release for QC / dissolution testing).
Excipients
No proprietary excipient used
The novel excipient poloxamer 338 (P338) is used in the final G001 clinical formulation. Following both an in-vitro mammalian chromosome aberration and an Ames test, it was considered to be non-genotoxic with no evidence for mutagenicity. Further P338 fertility, genotoxicity and development studies have been conducted with no negative effects, in addition to a 6-week and 9-month minipig repeat-dose toxicity study. No adverse local or systemic toxicity was reported in the minipigs at 100mg/month (Margin of Exposure:19).
No residual solvent used
Delivery device(s)
No delivery device
Publications
Jackson AG, Else LJ, Mesquita PM, et al. A compartmental pharmacokinetic evaluation of long-acting rilpivirine in HIV-negative volunteers for pre-exposure prophylaxis. Clin Pharmacol Ther. 2014;96(3):314-23. DOI: https://doi.org/10.1038/clpt.2014.118
Rilpivirine long-acting (RPV-LA) is a parenteral formulation enabling prolonged plasma exposure. We explored its multiple-compartment pharmacokinetics (PK) after a single dose, for pre-exposure prophylaxis. Sixty-six HIV-negative volunteers were enrolled: women received an intramuscular dose of 300, 600, or 1,200 mg, with plasma and genital levels measured to 84 days postdose; men receiving 600 mg had similar PK determined in plasma and rectum. Ex vivo antiviral activity of cervicovaginal lavage (CVL) was also assessed. After a single dose, RPV concentrations peaked at days 6-8 and were present in plasma and genital-tract fluid to day 84. Vaginal and male rectal tissue levels matched those in plasma. At the 1,200 mg dose, CVL showed greater antiviral activity, above baseline, at days 28 and 56. All doses were well tolerated. All doses gave prolonged plasma and genital-tract rilpivirine exposure. PK and viral inhibition of repeated doses will be important in further dose selection.
Mora-Peris B, Watson V, Vera JH, et al. Rilpivirine exposure in plasma and sanctuary site compartments after switching from nevirapine-containing combined antiretroviral therapy. J Antimicrob Chemother. 2014;69(6):1642-7. DOI: https://doi.org/10.1128/jvi.01912-19
As a long-acting formulation of the nonnucleoside reverse transcriptase inhibitor rilpivirine (RPV LA) has been proposed for use as preexposure prophylaxis (PrEP) and the prevalence of transmitted RPV-resistant viruses can be relatively high, we evaluated the efficacy of RPV LA to inhibit vaginal transmission of RPV-resistant HIV-1 in humanized mice. Vaginal challenges of wild-type (WT), Y181C, and Y181V HIV-1 were performed in mice left untreated or after RPV PrEP. Plasma viremia was measured for 7 to 10 weeks, and single-genome sequencing was performed on plasma HIV-1 RNA in mice infected during PrEP. RPV LA significantly prevented vaginal transmission of WT HIV-1 and Y181C HIV-1, which is 3-fold resistant to RPV. However, it did not prevent transmission of Y181V HIV-1, which has 30-fold RPV resistance in the viruses used for this study. RPV LA did delay WT HIV-1 dissemination in infected animals until genital and plasma RPV concentrations waned. Animals that became infected despite RPV LA PrEP did not acquire new RPV-resistant mutations above frequencies in untreated mice or untreated people living with HIV-1, and the mutations detected conferred low-level resistance. These data suggest that high, sustained concentrations of RPV were required to inhibit vaginal transmission of HIV-1 with little or no resistance to RPV but could not inhibit virus with high resistance. HIV-1 did not develop high-level or high-frequency RPV resistance in the majority of mice infected after RPV LA treatment. However, the impact of low-frequency RPV resistance on virologic outcome during subsequent antiretroviral therapy still is unclear.
IMPORTANCE The antiretroviral drug rilpivirine was developed into a long-acting formulation (RPV LA) to improve adherence for preexposure prophylaxis (PrEP) to prevent HIV-1 transmission. A concern is that RPV LA will not inhibit transmission of drug-resistant HIV-1 and may select for drug-resistant virus. In female humanized mice, we found that RPV LA inhibited vaginal transmission of WT or 3-fold RPV-resistant HIV-1 but not virus with 30-fold RPV resistance. In animals that became infected despite RPV LA PrEP, WT HIV-1 dissemination was delayed until genital and plasma RPV concentrations waned. RPV resistance was detected at similar low frequencies in untreated and PrEP-treated mice that became infected. These results indicate the importance of maintaining RPV at a sustained threshold after virus exposure to prevent dissemination of HIV-1 after vaginal infection and low-frequency resistance mutations conferred low-level resistance, suggesting that RPV resistance is difficult to develop after HIV-1 infection during RPV LA PrEP.
Ford N, Lee J, Andrieux-Meyer I, Calmy A: Safety, efficacy, and pharmacokinetics of rilpivirine: systematic review with an emphasis on resource-limited settings. HIV AIDS (Auckl). 2011;3:35-44. doi: https://doi.org/10.2147/hiv.s14559. Epub 2011 Apr 28.
The vast majority of people living with human immunodeficiency virus (HIV)/acquired immune deficiency syndrome reside in the developing world, in settings characterized by limited health budgets, critical shortages of doctors, limited laboratory monitoring, a substantial burden of HIV in children, and high rates of coinfection, in particular tuberculosis. Therefore, the extent to which new antiretrovirals will contribute to improvements in the management of HIV globally will depend to a large extent on their affordability, ease of use, low toxicity profile, availability as pediatric formulations, and compatibility with tuberculosis and other common drugs. We undertook a systematic review of the available evidence regarding drug interactions, and the efficacy and safety of rilpivirine (also known as TMC-278), and assessed our findings in view of the needs and constraints of resource-limited settings. The main pharmacokinetic interactions relevant to HIV management reported to date include reduced bioavailability of rilpivirine when coadministered with rifampicin, rifabutin or acid suppressing agents, and reduced bioavailability of ketoconazole. Potential recommendations for dose adjustment to compensate for these interactions have not been elaborated. Trials comparing rilpivirine and efavirenz found similar outcomes up to 96 weeks in intent-to-treat analysis; failure of rilpivirine was mainly virological, whereas failure among those exposed to efavirenz was mainly related to the occurrence of adverse events. Around half of the patients who fail rilpivirine develop non-nucleoside reverse transcriptase inhibitor resistance mutations. The incidence of Grade 2-4 events was lower for rilpivirine compared with efavirenz. Grade 3-4 adverse events potentially related to the drugs were infrequent and statistically similar for both drugs. No dose-response relationship was observed for efficacy or safety, and the lowest dose (25 mg) was selected for further clinical development. The potential low cost and dose of the active pharmaceutical ingredient means that rilpivirine can potentially be manufactured at a low price. Moreover, its long half-life suggests the potential for monthly dosing via nonoral routes, with promising early results from studies of a long-acting injectable formulation. These characteristics make rilpivirine an attractive drug for resource-limited settings. Future research should assess the potential to improve robustness and assess the clinical significance of interaction with antituberculosis drugs.
Azijn H, Tirry I, Vingerhoets J, de Bethune MP, Kraus G, Boven K, Jochmans D, Van Craenenbroeck E, Picchio G, Rimsky LT: TMC278, a next-generation nonnucleoside reverse transcriptase inhibitor (NNRTI), active against wild-type and NNRTI-resistant HIV-1. Antimicrob Agents Chemother. 2010 Feb;54(2):718-27. doi: https://doi.org/10.1128/aac.00986-09. Epub 2009 Nov 23.
Nonnucleoside reverse transcriptase inhibitors (NNRTIs) have proven efficacy against human immunodeficiency virus type 1 (HIV-1). However, in the setting of incomplete viral suppression, efavirenz and nevirapine select for resistant viruses. The diarylpyrimidine etravirine has demonstrated durable efficacy for patients infected with NNRTI-resistant HIV-1. A screening strategy used to test NNRTI candidates from the same series as etravirine identified TMC278 (rilpivirine). TMC278 is an NNRTI showing subnanomolar 50% effective concentrations (EC50 values) against wild-type HIV-1 group M isolates (0.07 to 1.01 nM) and nanomolar EC50 values against group O isolates (2.88 to 8.45 nM). Sensitivity to TMC278 was not affected by the presence of most single NNRTI resistance-associated mutations (RAMs), including those at positions 100, 103, 106, 138, 179, 188, 190, 221, 230, and 236. The HIV-1 site-directed mutant with Y181C was sensitive to TMC278, whereas that with K101P or Y181I/V was resistant. In vitro, considerable cross-resistance between TMC278 and etravirine was observed. Sensitivity to TMC278 was observed for 62% of efavirenz- and/or nevirapine-resistant HIV-1 recombinant clinical isolates. TMC278 inhibited viral replication at concentrations at which first-generation NNRTIs could not suppress replication. The rates of selection of TMC278-resistant strains were comparable among HIV-1 group M subtypes. NNRTI RAMs emerging in HIV-1 under selective pressure from TMC278 included combinations of V90I, L100I, K101E, V106A/I, V108I, E138G/K/Q/R, V179F/I, Y181C/I, V189I, G190E, H221Y, F227C, and M230I/L. E138R was identified as a new NNRTI RAM. These in vitro analyses demonstrate that TMC278 is a potent next-generation NNRTI, with a high genetic barrier to resistance development.
Lade JM, Avery LB, Bumpus NN: Human biotransformation of the nonnucleoside reverse transcriptase inhibitor rilpivirine and a cross-species metabolism comparison. Antimicrob Agents Chemother. 2013 Oct;57(10):5067-79. doi: https://doi.org/10.1128/aac.01401-13. Epub 2013 Aug 5
Rilpivirine is a nonnucleoside reverse transcriptase inhibitor used to treat HIV-1. In the present study, the pathways responsible for the biotransformation of rilpivirine were defined. Using human liver microsomes, the formation of two mono- and two dioxygenated metabolites were detected via ultra high-performance liquid chromatography-tandem mass spectrometry (UHPLC-MS/MS). Mass spectral analysis of the products suggested that these metabolites resulted from oxygenation of the 2,6-dimethylphenyl ring and methyl groups of rilpivirine. Chemical inhibition studies and cDNA-expressed cytochrome P450 (CYP) assays indicated that oxygenations were catalyzed primarily by CYP3A4 and CYP3A5. Glucuronide conjugates of rilpivirine and a monomethylhydroxylated metabolite of rilpivirine were also detected and were found to be formed by UDP-glucuronosyltransferases (UGTs) UGT1A4 and UGT1A1, respectively. All metabolites that were identified in vitro were detectable in vivo. Further, targeted UHPLC-MS/MS-based in vivo metabolomics screening revealed that rilpivirine treatment versus efavirenz treatment may result in differential levels of endogenous metabolites, including tyrosine, homocysteine, and adenosine. Rilpivirine biotransformation was also assessed across species using liver microsomes isolated from a range of mammals, and the metabolite profile identified using human liver microsomes was largely conserved for both oxidative and glucuronide metabolite formation. These studies provide novel insight into the metabolism of rilpivirine and the potential differential effects of rilpivirine- and efavirenz-containing antiretroviral regimens on the endogenous metabolome.
Van Klooster G. Hoeben E. Borghys H. et al. Pharmacokinetics and Disposition of Rilpivirine (TMC278) Nanosuspension as a long-acting injectable antiretroviral formulation. Antimicrob Agents Chemother. 2010; 54 (50066-4804/10/$12.00): 2042-2050. doi: https://doi.org/10.1128/AAC.01529-09
The next-generation human immunodeficiency virus type 1 (HIV-1) nonnucleoside reverse transcriptase inhibitor rilpivirine (TMC278) was administered in rats and dogs as single intramuscular (IM) or subcutaneous (SC) injections, formulated as a 200-nm nanosuspension. The plasma pharmacokinetics, injection site concentrations, disposition to lymphoid tissues, and tolerability were evaluated in support of its potential use as a once-monthly antiretroviral agent in humans. Rilpivirine plasma concentration-time profiles showed sustained and dose-proportional release over 2 months in rats and over 6 months in dogs. The absolute bioavailability approached 100%, indicating a complete release from the depot, in spite of rilpivirine concentrations still being high at the injection site(s) 3 months after administration in dogs. For both species, IM administration was associated with higher initial peak plasma concentrations and a more rapid washout than SC administration, which resulted in a stable plasma-concentration profile over at least 6 weeks in dogs. The rilpivirine concentrations in the lymph nodes draining the IM injection site exceeded the plasma concentrations by over 100-fold 1 month after administration, while the concentrations in the lymphoid tissues decreased to 3- to 6-fold the plasma concentrations beyond 3 months. These observations suggest uptake of nanoparticles by macrophages, which generates secondary depots in these lymph nodes. Both SC and IM injections were generally well tolerated and safe, with observations of a transient inflammatory response at the injection site. The findings support clinical investigations of rilpivirine nanosuspension as a long-acting formulation to improve adherence during antiretroviral therapy and for preexposure prophylaxis.
Mc Crudden MTC, Larrañeta E, Clark A et al. Design, formulation and evaluation of novel dissolving microarray patches containing a long-acting rilpivirine nanosuspension. J Control Release 2018; 292: 119–29. doi: https://doi.org/10.1016/j.jconrel.2018.11.002
One means of combating the spread of human immunodeficiency virus (HIV) is through the delivery of long-acting, antiretroviral (ARV) drugs for prevention and treatment. The development of a discreet, self-administered and self-disabling delivery vehicle to deliver such ARV drugs could obviate compliance issues with daily oral regimens. Alternatives in development, such as long-acting intramuscular (IM) injections, require regular access to health care facilities and disposal facilities for sharps. Consequently, this proof of concept study was developed to evaluate the use of dissolving microarray patches (MAPs) containing a long-acting (LA) nanosuspension of the candidate ARV drug, rilpivirine (RPV). MAPs were mechanically strong and penetrated skin in vitro, delivering RPV intradermally. In in vivo studies, the mean plasma concentration of RPV in rats (431 ng/ml at the Day 7 time point) was approximately ten-fold greater than the trough concentration observed after a single-dose in previous clinical studies. These results are the first to indicate, by the determination of relative exposures between IM and MAP administration, that larger multi-array dissolving MAPs could potentially be used to effectively deliver human doses of RPV LA. Importantly, RPV was also detected in the lymph nodes, indicating the potential to deliver this ARV agent into one of the primary sites of HIV replication over extended durations. These MAPs could potentially improve patient acceptability and adherence to HIV prevention and treatment regimens and combat instances of needle-stick injury and the transmission of blood-borne diseases, which would have far-reaching benefits, particularly to those in the developing world.
Additional documents
No documents were uploaded
Collaborate for development
Consider on a case by case basis, collaborating on developing long acting products with potential significant public health impact, especially for low- and middle-income countries (LMICs), utilising the referred to long-acting technology
Share technical information for match-making assessment
Provide necessary technical information to a potential partner, under confidentiality agreement, to enable preliminary assessment of whether specific medicines of public health importance in LMICs might be compatible with the referred to long-acting technology to achieve a public health benefit
Work with MPP to expand access in LMICs
In the event that a product using the referred to long-acting technology is successfully developed, the technology IP holder(s) will work with the Medicines Patent Pool towards putting in place the most appropriate strategy for timely and affordable access in low and middle-income countries, including through licensing